How Mobile Devices Impact Patient Satisfaction
Patient satisfaction is an important metric for any healthcare provider. It serves as an indicator of the quality of care, as well as the efficiency and personability of a provider and their office. Within the past year, one in eight patients left a practice, and approximately one-third of patients could switch within the next few years. If a practice loses a patient due to dissatisfaction, it could lose $200,000 in revenue over its lifetime. Satisfied patients are more likely to reach out to other people and recommend the practice, while dissatisfied patients can deter others people from coming to your practice.
Patient satisfaction is also being measured by the Clinician & Group Consumer Assessment of Health Providers and Systems (CG-CAHPS), which is increasingly linking patient satisfaction to reimbursement.
Healthcare providers are seeking actionable ways to improve patient satisfaction. Two key ways to improve patient satisfaction include:
- Staff Training: Your staff is the face of your practice. They are usually the first and last points of contact a patient will have. Staff members with a friendly, welcoming demeanor are more likely to result in satisfied patients. Additionally, staff members who are efficient and capable will make the patient experience a smooth one.
- Wait Times: Approximately 60 percent of patients are not willing to hold on the phone for more than a minute. Patients left waiting on the phone or in the waiting room before their appointments are less likely to feel satisfied with their experience.
Mobile devices are ubiquitous, but have you thought about how smartphones and tablets can be used to improve patient satisfaction? Often referred to as mHealth in the medical field, keep reading to learn more about how mobile devices are transforming healthcare.
Uses for Mobile Devices in Healthcare
Mobile devices can be used across nearly any healthcare setting for a variety of purposes. Approximately 90 percent of healthcare organizations have implemented or are planning to implement some kind of mobile device initiative. Here are three of the common uses if mobile devices in healthcare.
1. Staff Communication
Communication is a critical part of providing quality patient care. Providers need to be able to share information with one another across entire facilities. Mobile devices offer real-time access to that vital information.
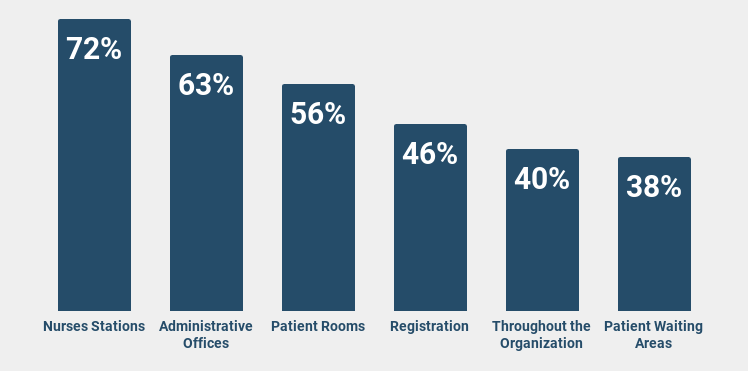
Some of the most common uses of mobile devices for staff communication include nurse stations (72 percent), administrative offices (63 percent), and registration (46 percent). Additionally, 40 percent of organizations report using mobile devices throughout their organizations. Smartphones are the most commonly used mobile device, with 77 percent of healthcare survey respondents saying they use them in their organization. Healthcare organizations also use mobile devices like tablets and pagers.
Access to mobile devices enables healthcare staff members to communicate via email, text, voice calling and video calling. It also allows access to electronic health records (EHRs) and clinical decision support tools. This access to information and the ability to rapidly communicate it is a powerful tool for practicing evidence-based medicine.
2. Patient Engagement
Patient engagement is an important metric with plenty of room for improvement. Healthcare leaders and providers report that they consider just 34 percent of their patients highly engaged. Mobile devices can be an integral piece of the patient engagement puzzle.
Nearly all patients will have some kind of mobile device, whether a smartphone, tablet or both. They can use those mobile devices to access their health records. Approximately 75 percent of patients say easy access to their electronic health information would improve their ability to communicate with providers. Additionally, 80 percent of people who have access to their electronic health information will use it.
For example, providers can give patients access to EHRs through tools like a patient portal. This type of secure accessibility can result in patient engagement with a measurable impact. More engaged patients are more likely to have positive outcomes. In fact, 93 percent of physicians report that they think mHealth apps can be linked to improved outcomes.
3. Patient Education
Approximately 50 percent of Americans are healthcare illiterate, which means they do not understand what to do with healthcare information. That means there is a significant opportunity to employ patient education strategy.
Empowered with an understanding of their healthcare information, people can better take care of themselves. Physicians, nurses and other support staff play an important role in educating patients, and they can do this through many different methods. Mobile devices can play a big part in providing that education.
Of the healthcare organizations implementing mHealth programs, 64 percent reported the delivery of educational apps and materials related to patient care was a key motivator. Physicians could use a mobile device, like a tablet, to review imaging test results with a patient. Healthcare organizations could place tablets with mHealth apps and other educational material in patient rooms. Additionally, patients could access a healthcare organization’s secure network on their own devices to view their medical records and learn more about their own health.
Information is a powerful tool, but people need access to it to put it to use. Mobile devices are an integral part of most people’s lives, which gives healthcare providers the opportunity to offer access to vital information, as well as help patients understand it.
How Mobile Devices Can Help Patient Satisfaction
The impact of mobile technology in healthcare is far-reaching. Not only does it make it easier for providers to do their jobs, but it can also do a lot to improve patient satisfaction. Here are three ways mobile devices can make a difference in your organization’s overall patient satisfaction.
1. Improved Communication
Mobile devices improve communication in two major ways:
- Between the members of a patient’s care team
- Between providers and their patients
Half of the healthcare organizations that have implemented mobile device initiatives reported improved communication across departments, while 45 percent said improved communication between staff and patients. Communication between care providers can make patient care more efficient. Everyone involved in a patient’s care is on the same page about the patient’s condition and the approach to treatment.
Efficient care is inevitably going to affect patient satisfaction. Likewise, communication between providers and patients is going to be a major part of the provider-patient relationship. Mobile devices empower physicians and other clinical workers an educational tool while they are caring for a patient in person.
A properly implemented mobile device program also gives providers and patients a secure way to communicate outside of the healthcare organization. If providers offer patients access to convenient communication options, they are more likely to build a strong relationship, which leads to more satisfied patients.
2. Increased Provider Efficiency
Patients are increasingly adopting a consumer mindset in the healthcare space, particularly as they shoulder more of the cost of their care. Efficiency is going to stand out to patients and engender their loyalty. Many patients have multiple people working on their care team. The combined medical knowledge of this team is a great benefit, but it also opens the door to miscommunication and gaps in care.
When the members of a clinical care team are unable to communicate effectively with one another, the care process becomes inefficient — and patients will notice. If they need to answer the same set of questions for multiple different people, their satisfaction with their care is going to decrease. Mobile devices can help close those gaps in communication and improve overall care efficiency.
For example, healthcare organizations included a more efficient transfer of information and improved transparency across departments as two tangible benefits of mobile device programs.
3. Added Convenience
Convenience, like efficiency, is a significant factor in patient satisfaction. People do not want to wait on hold on the phone to make an appointment or ask their provider a question. They do not want to have to drive and pick up a physical copy of their medical records. They do not want to fill out paperwork in the office while they wait for their appointment.
Nearly half of patients — 42 percent — want the option to book appointments digitally, yet just 17 percent have access to online booking. The time spent doing any of those errands above is going to affect patient satisfaction. Mobile devices can help reduce or eliminate many of these issues.
For example, access to a patient portal allows patients to schedule appointments and ask providers questions from their mobile device. It also allows them to access digital copies of their medical records and fill out registration paperwork online before their appointments. Patient portals can even offer people the option to pay bills online, rather than mailing a check or calling to pay over the phone.
Should You Be Concerned About Using Technology for Patient Satisfaction?
Despite all the benefits of mobile devices in healthcare, the use of this technology is not without risk. Data security and patient privacy is always a concern when handling sensitive information. Additionally, the cost of a new technology initiative and the logistics of implementing it effectively can be daunting. Here are three of the top concerns regarding mobile device use that providers should be aware of.
1. HIPAA
Healthcare organizations implementing mobile health strategies reported data privacy (67 percent) and security and compliance (66 percent) as top concerns. Mobile devices mean healthcare providers can access sensitive patient data from anywhere at any time, which does mean there is a risk for exposing or compromising that data.
While that is true, it is certainly possible to implement a HIPAA-compliant mobile device program. Conducting a thorough risk assessment is the first step to ensuring HIPAA compliance. This type of assessment should cover an organization’s IT infrastructure. Are all of the necessary defense strategies, like firewalls and password protection, in place? The risk assessment also needs to cover an organization’s mobile device policies and procedures.
Any risks uncovered during this assessment need to be quickly and adequately addressed. Additionally, you should continue to conduct risk assessments on a regular basis. Threats to data security are not static, so healthcare organizations need to evolve and update their strategies to keep up with the latest security threats.
2. Implementation
Implementation of a mHealth program can be a lengthy and involved process. Nearly half of the healthcare organizations implementing mobile technology (41 percent) are concerned about inappropriate employee use. And, this is a valid concern. Insiders cause approximately 58 percent of private health information data breaches.
While that is a concerning statistics, proper implementation of policies and security protocols can mitigate insider risk, which includes user error and misuse of sensitive data. Understand the risk ahead of time, and strategically implement mHealth to reduce that risk. Start the program on a smaller scale, perhaps in just one part of the organization. Measure the results. What is working? What isn’t? Refine the program before beginning a larger scale implementation.
Along the way, work to gain provider and employee buy-in. The more engaged they are, the more likely the program is to be successful. You should also work closely with your IT team to ensure each step of the implementation is done with the right security measures in place. While effective implementation can be a challenge, the benefits of increased patient satisfaction can be well worth it for a healthcare organization.
3. Cost
Of all the healthcare organizations not planning to implement a mobile device initiative, 61 percent cited the price as a major barrier. While mHealth certainly represents a significant investment, healthcare providers must weight the cost against the benefits of a mobile initiative. If cost still remains a primary concern, there are ways to save while implementing this type of project.
For example, many healthcare providers implement a bring your own device (BYOD) program. This type of program allows healthcare providers to bring their own devices, which they already own, to work. With this type of program, a healthcare facility or practice can save on the upfront cost of acquiring devices and maintaining them.
While there is certainly a potential for cost savings, healthcare organizations need to conduct a cost analysis that takes into account both direct and indirect costs of a BYOD program. Implementation and training for this type of program is a direct cost. Potential security risks, such as the use of unapproved apps, are indirect costs for healthcare organizations. Whether an organization decides to pay directly for a mHealth program or go the BYOD route, proper planning, training and implementation can help ensure the benefits outweigh the cost and risk.
Choose ICANotes to Increase Patient Satisfaction
Digital health is becoming increasingly important in the healthcare space. If your behavioral health practice is looking to leverage technology to be more efficient — and, by extension, improve patient satisfaction — ICANotes offers an EHR solution tailored explicitly for behavioral health. Features include charting, billing, practice management, security and a patient portal.
ICANotes is available for download on iPhones, iPads and Android devices, so it can easily become a part of your practice’s mobile device initiative. Empower your behavioral health practice with seamless, secure communication. Your patients — and your bottom line — will thank you.
Related Posts:
2018 Updates to the EHR Incentive Program
How Electronic Health Records Are Improving Patient Care
How to Give Patients Access to Their Mental Health Records
Are Mental Health Record Guidelines the Same for Every State?