Blog > Documentation > Beginners Guide to Mental Health Notes
Beginners Guide to Mental Health Notes
Keeping clear, consistent mental health notes is critical for both client care and insurance compliance. Whether you're a new clinician or opening your own practice, understanding the different types of notes required is essential. From progress notes to treatment plans, each note plays a role in supporting effective therapy and meeting documentation standards.

Last Updated: May 16, 2025

What You'll Learn
-
The key types of mental health notes and when to use each one
-
What to include in progress notes, treatment plans, and discharge summaries
-
Common note-taking mistakes to avoid in clinical documentation
-
Time-saving tips and tools for writing clear, compliant notes faster
Counselors, psychologists, clinical social workers, and other behavioral health professionals need to write notes when they see clients. Mental health notes, such as assessments and progress notes, help clinicians document the diagnosis and treatment of clients. These notes keep behavioral health professionals from having to start from scratch every time they meet with a client.
Mental health notes also save clinicians from needing to rely on their memory for each session. Some behavioral health professionals may see over 20 clients per week, so trying to remember each individual's mood, thoughts and feelings without writing these details down is nearly impossible. This is especially true if some clients come into the office less often than others, leaving days or weeks between their visits.
Mental health notes are also critical for insurance reimbursement. Insurance companies may need to see your progress notes to determine whether they will accept or deny a claim. Your notes can prove to insurers that your services are necessary and effective.
If you're about to open a private practice or are new to the behavioral health field, it helps to know the various types of mental health notes you might use when treating clients. In this beginner's guide, we'll explore some common types of mental health notes, what they include, and why clinicians use them.
Download Our Guide to Writing Better, Faster Clinical Notes
Streamline your progress notes, avoid documentation pitfalls, and stay compliant with practical templates, note formats (SOAP, DAP, BIRP), and time-saving tips to write high-quality, defensible notes faster.
What Are Mental Health Notes?
Mental health notes refer to the different types of notes a clinician might create during or after an appointment with a client. In general, mental health notes typically include the client's diagnosis, their current status, anything they reveal during the session, the clinician's assessment, a treatment plan and any other relevant health information.
As the American Psychological Association (APA) states, behavioral health professionals have an ethical and professional responsibility to maintain accurate records. Mental health notes are a necessity in the behavioral health field because they enable clinicians to do the following:
- Provide high-quality care: Mental health notes allow you to monitor a client's progress without relying only on your memory. Your notes can also help you connect a client's stories, behaviors, symptoms, thoughts and feelings to form a more accurate diagnosis. If something isn't working in treatment, you can use your notes to guide your decisions and adjust a client's treatment plan accordingly. All of these factors can help you treat clients effectively.
- Remember clients: You can refer to a client's notes whenever you need a reminder about a specific piece of information, enabling you to provide better care. Mental health notes also keep you updated and informed about a client's medications and overall health, which can help you factor in other health components that may be influencing their mental wellness.
- Get reimbursed: Your mental health notes provide the proof you need to get paid by insurance companies for your services. For example, the Centers for Medicare and Medicaid Services require documentation to reflect medical necessity. Accuracy is vital when billing clients or insurers, and note-taking helps you share specific details error-free.
- Coordinate care: Mental health notes facilitate care coordination between providers. By storing your notes in an electronic health record (EHR) system, you can easily and securely share your client's information with their family physician or other health care professionals so they can make informed decisions. Notes also prevent clients from undergoing the same tests twice, which saves them time, money and aggravation.
- Protect yourself: By keeping accurate, detailed notes, you create evidence of what a client's diagnosis is and how you treated them. If a client decides to file a lawsuit or complaint with the licensing board, you may be able to use your notes to support your case.
Behavioral health professionals document various notes to comply with ethical guidelines, deliver high-quality service and get reimbursed for their work. The following types of notes are critical in maintaining accurate client records and providing the best care possible:
1. Assessments
Clinicians administer assessments to learn about clients, form diagnoses and devise treatment plans. Usually, behavioral health professionals assess clients during their initial sessions, but they should re-evaluate clients periodically and make adjustments to their treatment plans as needed.
The clinical interview is an assessment example. During the clinical interview, the behavioral health professional asks the client questions about their medical history and current symptoms. For example, a clinician might ask a client with depression how long they've been experiencing symptoms and how it has affected their life. The clinician may also ask questions about the client's family history, childhood and relationships to get a clearer picture of their mental health and diagnostic clues.
Behavioral health clinicians might also use biopsychosocial assessments to understand clients' health backgrounds and current conditions. A biopsychosocial assessment is a comprehensive approach that helps mental health professionals evaluate clients holistically, considering biological, psychological and social factors. Biopsychosocial assessments typically include the following information:
- Current symptoms
- Medical history
- Mental health history
- Current and past relationships
- Employment and educational background
- Legal issues
- Substance abuse history
You might choose an assessment based on what a client's issues are and what you need to understand about them. Initial assessments are typically required to prove medical necessity and get reimbursed by insurers and government programs.
2. Psychotherapy Notes
Psychotherapy notes are a clinician's private notes that they take during sessions. Psychotherapy notes are not required for reimbursement, and they must be kept confidential. These notes are stored separately from clients' records and are meant only to be seen by the clinician who writes them.
Clients do not have a right to read your psychotherapy notes under the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule. However, if they ask to see your psychotherapy notes regarding one of their sessions, you have a right to share them.
Since psychotherapy notes are optional, they do not need to follow a particular format. The purpose of psychotherapy notes is to help you do your job better. Depending on your needs, your psychotherapy notes may include thoughts, feelings, and observations you make during a session with a client. You can include whatever is necessary to help you treat clients.
3. Progress Notes
Progress notes are critical for receiving reimbursement and communicating a client's treatment plan to other staff members. Unlike psychotherapy notes, progress notes are meant to be shared with appropriate parties, such as other health care providers and insurers. These notes include details about your client's current status and progress. They should be concise, accurate, legible, and compliant with HIPAA.
Progress notes can follow several formats. Common progress note formats include Subjective, Objective, Assessment, Plan (SOAP) and Behavior, Intervention, Response, Plan (BIRP). You can choose the best format that works for you and your practice.
It's best to write progress notes immediately after a session with a client while the meeting is still fresh in your mind. You can refer to these notes in the future to refresh your memory before another appointment. You can also use progress notes to fill out insurance claims accurately.
4. Treatment Plan
A treatment plan is a detailed map used to guide clients toward the goals they set in therapy. Progress against the treatment plan is typically document in a client's progress notes. Clinicians usually create treatment plans during their initial sessions with clients, working with them to set goals and objectives. Treatment plans often include:
- Demographic information.
- Mental health history.
- Diagnostic summary.
- Goals and timelines.
- Services to be provided and their frequency.
Treatment plans help counselors get approved by insurers to continue providing services for clients. Some insurance companies require regular treatment plan reviews and updates.
5. Discharge Summary
Behavioral health professionals create discharge summaries when clients complete a treatment program or are released from the hospital. A discharge summary includes the reason a client sought treatment, the services provided, the client's condition upon discharge, and a follow-up plan.
Discharge summaries are important for communicating aftercare instructions to patients and their families. Discharge summaries also convey a client's follow-up plan to other health care providers. Regarding reimbursement, discharge summaries may be required depending on the client's insurance carrier.
How to Write Concise Mental Health Notes
Writing mental health notes can seem like a time-consuming task. Many clinicians put off writing notes either because they can't find enough time in their workday or they haven't formed a note-taking routine. Others might add too much detail to their notes in fear they'll leave out something important.
The good news is notes do not have to be textbook-sized documents. Although they do need to include certain details, they should still be as brief and easy to read as possible. Here's how to write concise mental health notes and save time in the process:
- Focus on key details: Clients might share a lot of different information during a session, and some details may not be relevant. To keep yourself from feeling overwhelmed, plan to focus only on the most important information about a session, such as aspects related to the client's treatment plan.
- Follow a format: Following a format, such as SOAP or BIRP, helps you concentrate on essential elements needed for getting reimbursement and providing excellent care. Choose a format that works for you, and keep each section as brief as possible or only a few sentences long.
- Set a timer: Writing mental health notes should take about 10 minutes per session. If you discover it's taking you more than 15 minutes to write notes, think about areas that are taking up too much of your time, and consider ways to be more concise.
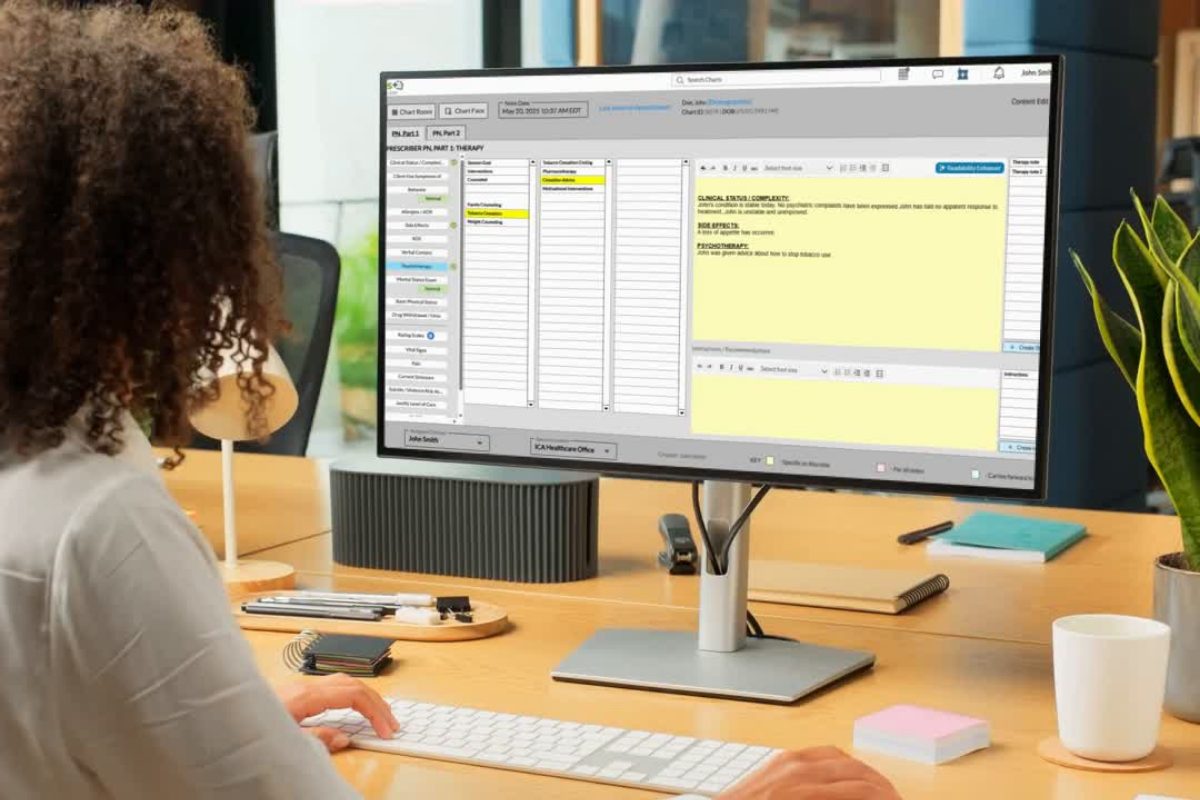
Use an efficient electronic health record (EHR) system: An EHR system like ICANotes allows you to use customizable menu-based templates, so you can quickly document therapy sessions with minimal typing. You can use ICANotes to generate progress notes, treatment plans, discharge summaries and other types of mental health notes in just a few minutes.
Avoiding Common Mental Health Note Mistakes
You can't avoid writing mental health notes as a counselor, but you can steer clear of mistakes. Although every clinician will have their own note-taking preferences, there are certain traps every behavioral health professional should try to bypass. Here's how to avoid common note-taking mistakes:
- Create legible digital notes: Mental health notes must be legible for sharing with other health care providers and staff members. You also want to have an easy time reading your own notes to provide client care. To prevent readability issues, create notes electronically in an EHR system for behavioral health and avoid handwriting your notes.
- Be clear and concise: Avoid using vague language, abbreviations and shorthand when creating mental health notes, and try to be as clear and concise as possible. There's no need to include unnecessary details. It's best to be specific and to the point. This will help prevent confusion between staff members and enable seamless care coordination.
- Avoid cutting corners: Every note needs to include certain details like the client's name, your name, the date and the time. You should also sign your notes electronically. By ensuring you complete every vital step, you'll save yourself from ethical or legal issues down the road.
- Know the laws and ethical guidelines: Always keep up to date on record-keeping laws and ethical guidelines in your state. Also, be sure to understand the note-taking requirements set by third-party payers. Knowing these requirements will help you include the most critical information in your notes and keep you from running into issues.
Schedule in time every day: Set aside time to complete documentation tasks and stick to your routine. You'll want to keep sessions fresh in your mind and avoid falling behind. Try to jot down each session's essential elements either during therapy or immediately after the appointment and then add them to your EHR. Ideally, you should set aside around 10 to 15 minutes after each session to take notes.
Write Better and Faster Mental Health Notes with ICANotes
Crafting high-quality mental health documentation doesn't have to be a time-consuming burden. ICANotes transforms note-taking into a fast, intuitive, and clinically robust process designed specifically for behavioral health providers.
1. Menu-driven, narrative-style notes
Skip the endless typing and instead select pre-written, clinically validated phrases through a smart menu-based interface. These clicks generate polished, paragraph-style notes that read naturally and resonate with both clients and auditors. It’s quality documentation, with about 80% less effort.
2. Templates tailored for behavioral health
Choose from a rich library of templates: progress notes, soap/DAP/BIRP formats, treatment plans, MSEs, and more, fully customizable to fit your specialty. They're built for completeness, ensuring you don’t miss key components like risk assessment or treatment interventions.
3. Compliance and coding support built-in
Forget looking up CPT and ICD codes manually. ICANotes automatically maps your selected phrases to accurate billing codes and structures documentation in audit-ready formats. That means fewer errors and more efficient reimbursement processes.
4. Narrative depth, audit-ready structure
While it enables faster documentation, ICANotes doesn't compromise clarity or human context. Notes maintain a narrative flow, ideal for conveying clinical nuance, while still meeting payer and legal requirements.
5. Significant time and ROI benefits
Clinicians report reducing documentation time from ~30 minutes to just 5. That frees up as much as 90 minutes daily—whether to see more clients, enhance care, or simply reclaim personal time
With ICANotes, you're not just charting faster, you're charting smarter. If you would like to try ICANotes and see how it works for you, please request your free trial or schedule a live demo to learn more.
Schedule a Live Demo
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals—built to streamline documentation, improve compliance, and enhance patient care.
- Simplify clinical charting
- Stay organized with appointment scheduling
- Reduce no-shows with automated reminders
- Improve client engagement with a secure patient portal
- Provide flexible care with HIPAA-compliant telehealth
Simplify clinical charting
Stay organized with appointment scheduling
Reduce no-shows with automated reminders
Improve client engagement with a secure patient portal
Provide flexible care with HIPAA-compliant telehealth
Related Posts
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) from Aspen University and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care