Mental Status Exam
Cheat Sheet
Learn how to conduct a comprehensive mental status exam, understand its key components, and explore its role in diagnosing and tracking mental health conditions.

Last Updated: February 10, 2025


What You'll Learn
- The key components of a mental status exam and how they are assessed.
- Why mental status exams are essential for diagnosis and treatment planning.
- When and how to perform a mental status exam effectively.
- How different mental health professionals use mental status exams in practice.
A mental status exam is an assessment of a patient's cognitive and behavioral functioning. It’s based on the clinician’s observations and the client's subjective descriptions. You might think of a mental status exam as a psychiatrist’s version of a physical exam. Behavioral health professionals use mental status exams to create a picture of how a person looks in the present moment — not all of the time.
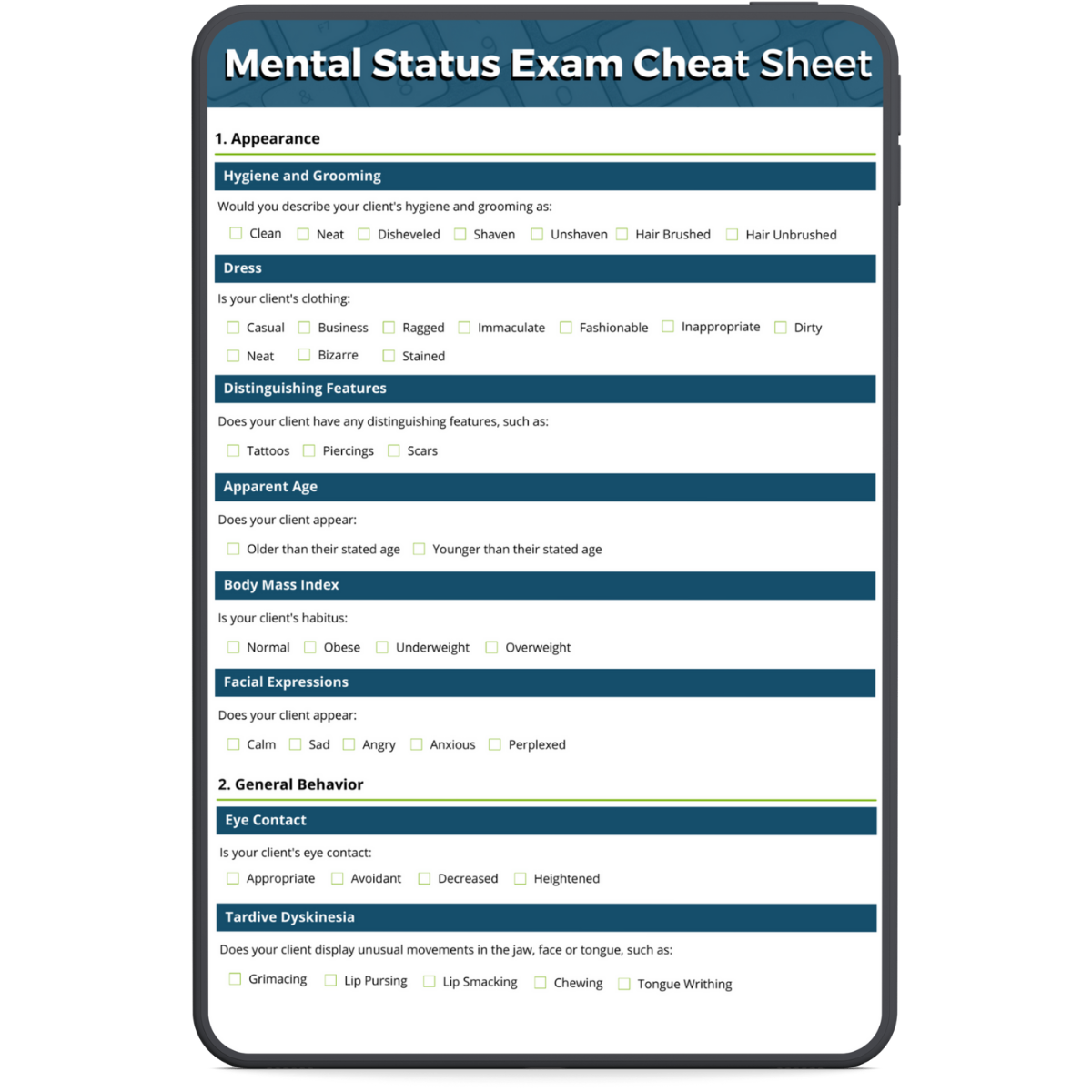
Download our
Mental Status Exam Cheat Sheet
Download our free mental health status exam cheat sheet to use as a handy reference when performing a mental status exam.
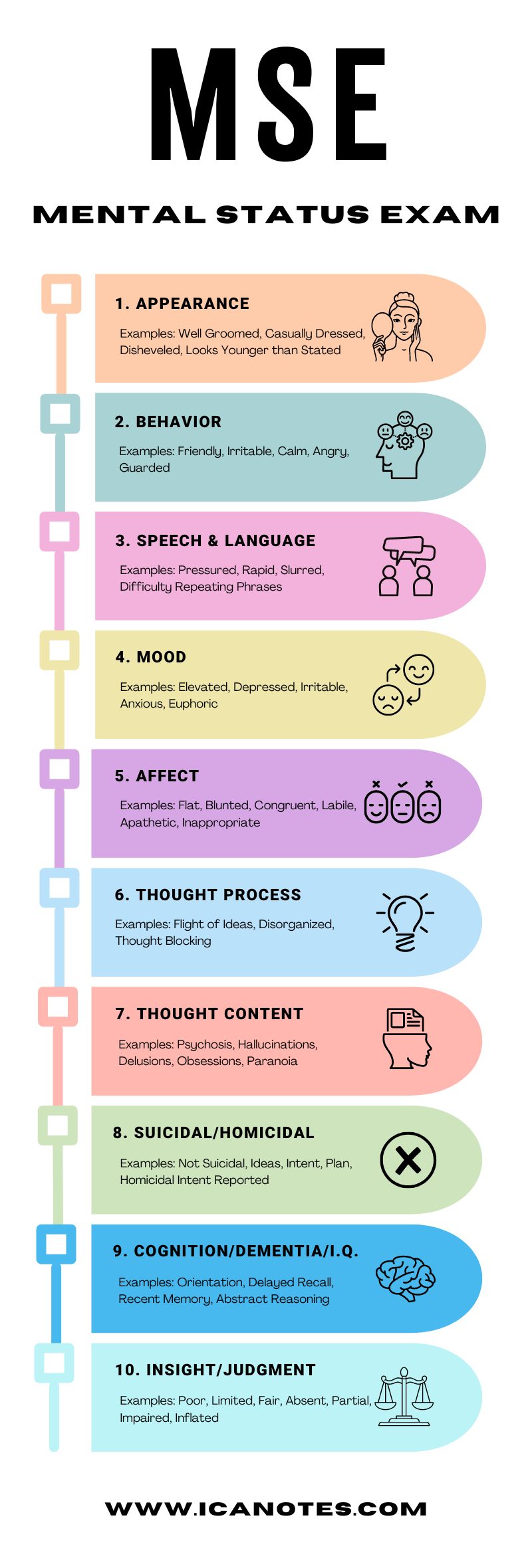
What are the Components of a Mental Status Exam?
- Appearance
- General behavior
- Speech and language
- Emotions
- Thought and perception
- Cognition
Why are Mental Status Exams Important?
In combination with family and personal histories, the mental status exam forms the foundation for a psychiatric diagnosis. Clinicians can also use mental status exams for the following reasons:
- To determine if certain issues are improving or getting worse
- To identify areas that need attention from a specialist
- To offer a snapshot of a client at a specific point in time and provide that information to another provider
When are Mental Status Exams Performed?
Mental status exams are often performed during the first one or two sessions with a client as part of the initial assessment and when reassessing their symptoms. Due to its visual elements, it should be performed in person and not over the phone. Mental status exams are instrumental in helping clinicians differentiate between various psychiatric and neurological disorders.
Typically, these exams are used for patients who have chronic, severe, or acute symptoms. A mental status exam aims to capture dysfunction, though you can still use it to confirm ordinary function for clients.
As a behavioral health professional, you may choose to complete regular mental status exams to identify progress or on an as-needed basis throughout the treatment process. Completing a mental status exam at the end of treatment can highlight the differences in a client's presentation and illustrate their growth. Keep our mental status exam cheat sheet handy to help guide your exam process.
Who Uses Mental Status Exams?
Although mental status exams have been an assessment tool mainly used in clinical psychology, psychiatry, and social work to examine patients with an altered mental status or evolving impairment of cognition, counselors and therapists can also use this type of exam as an informal way to gain information about a client’s cognitive and behavioral functioning. The counselor's findings can help them diagnose and treat a mental health disorder. Mental status exams also provide an excellent source of documentation to support a diagnosis.
How Do I Write a Mental Status Exam?
In private practice, you have the flexibility to create the sections you want to include in your mental status exam. When you are writing your mental status exam, review the typical sections, and identify which ones you believe will be useful to document during your intake assessments with clients. Keep in mind that some sections may be more or less relevant for specific clients.
To determine which portions to include in your mental status exam, consider your current clients. Would this apply to at least half of them? If so, it will likely be useful for you. If not, maybe you don't need to include it every time, and you can add it whenever necessary. You may also want to have an "other" section for topics that may come up during a mental status exam but do not fit in already established sections.
Mental Status Exam Checklist
To help you use a mental status exam as an assessment tool, we've created a mental status exam checklist. The following checklist is meant to be easy to read, so you can use it as a quick reference. Although you can customize a mental status exam to suit each client, you’ll generally want to focus on the categories in this mental status exam checklist:
1. Appearance
Appearance includes your observations of how a client looks initially and throughout the assessment. A client's appearance gives you an idea of their functioning level, their history, and the symptoms they're experiencing. Always look for signs of self-neglect and note anything unusual.
2. General Behavior
Describe how your client moves and behaves physically during the assessment. Always note if they are being hostile, uncooperative, or have inappropriate impulses.
3. Speech & Language
Consider how your client speaks and uses language. The amount a client speaks and how they talk can indicate a mental health issue such as depression or anxiety or a neurocognitive disorder.
Share this graphic by copying the following HTML code
[copy] <p><strong>www.icanotes.com</strong><br /><br /><a href='https://www.icanotes.com/2021/03/31/mental-status-exam-cheat-sheet/?fl_builder&fl_builder_ui'><img src='https://www.icanotes.com/wp-content/uploads/2021/03/MSE-infographic-2024-1.jpg' alt='MSE infographic 2024 (1)' width='800' /></a></p>
4. Emotions
Try to determine your client's emotional state by asking them how they feel and observing their facial expressions and body language.
5. Thought & Perception
Consider how your client's thoughts flow and connect and whether your client has a normal, linear thought process or if they go off-topic or make disorganized associations. Also, listen to what your client focuses on and find out if they're experiencing hallucinations. Always note hallucinations or the presence of delusions, and take appropriate action if a client expresses plans to carry out suicidal or homicidal ideation.
6. Cognition
When evaluating a client's cognition, clinicians commonly assess the person's alertness or level of consciousness, orientation, attention, concentration, and memory. If your client shows symptoms of a neurocognitive disorder, consider using additional tools such as the Mini-Mental State Examination or the Montreal Cognitive Assessment.
7. Environment
If part of your mental status exam includes assessing the client's living environment, you may want to describe their surroundings. Ask yourself the following:
- Have they made odd decisions, such as blocking doors or windows with furniture?
- Are there unusual decorations or wires that lead nowhere?
- Are they using any household objects inappropriately?
- Is their home extremely cluttered or dirty?
- Do they collect junk or garbage?
Mental Status Exam Example
Here is a brief mental status exam example:
- Appearance: The client is slouched and disheveled.
- General behavior: The client is uncooperative and has poor eye contact.
- Speech: The client speaks fast and soft.
- Emotions: The client states he feels "depressed and anxious."
- Thinking process: The client is incoherent and disorganized.
- Cognition: The client is focused and alert, and he performed well on working memory tests.
- Insight: The client displays poor insight.
- Judgment: The client shows fair judgment.
- Reliability: The client is unreliable because he gave false impressions of himself.
Start Your Free Trial of ICANotes
Accurate and efficient documentation is essential for delivering quality behavioral health care. ICANotes simplifies the process with a clinically robust EHR software designed specifically for mental health professionals.
Our intuitive system comes preloaded with comprehensive templates for every setting and discipline, allowing you to create:
✅ Discharge summaries
✅ Group therapy notes
✅ Initial assessments
✅ Progress notes
✅ Treatment plans
Experience the EHR that thinks like a clinician. Try ICANotes for free today!