Clinical notes are a vital part of behavioral health and therapy. They help track progress, determine diagnoses and can protect mental health professionals in malpractice lawsuits. Still, persistent myths surround behavioral therapy notes, how clinicians should write them and what you should or shouldn't include. Let's debunk these misconceptions so you can understand why you might wish to change your processes.
1. Notes Should Be as Brief as Possible
For many clients, their time with you is their only time to talk about everything they've been feeling or experiencing. They may share a lot of information during a clinical session, and you'll have to determine what is worth including in your notes. While you may want to keep your notes brief to save yourself time, it's best to include more details to ensure you don't miss information. Including relevant information in your notes helps you more effectively document your interactions with your clients.
While there's no reason to write a novella for each session, noting pertinent details can be helpful for several reasons. For example, documenting a client's stressors can help you create a treatment plan. Having this information in your notes serves as a reminder for you and the client, and justifies your treatment plan for any other mental health professionals who may read it. Documenting information like triggers in your notes also gives you things to follow up on in the future.
While it's a best practice to keep your notes concise for organization purposes, be sure you're not leaving out critical information in an attempt to keep your notes as brief as possible. If you're unsure about what to include, try using SOAP or BIRP note templates to focus your note writing. Using templates for your notes can help you find a balance between recording relevant information and keeping your notes succinct.
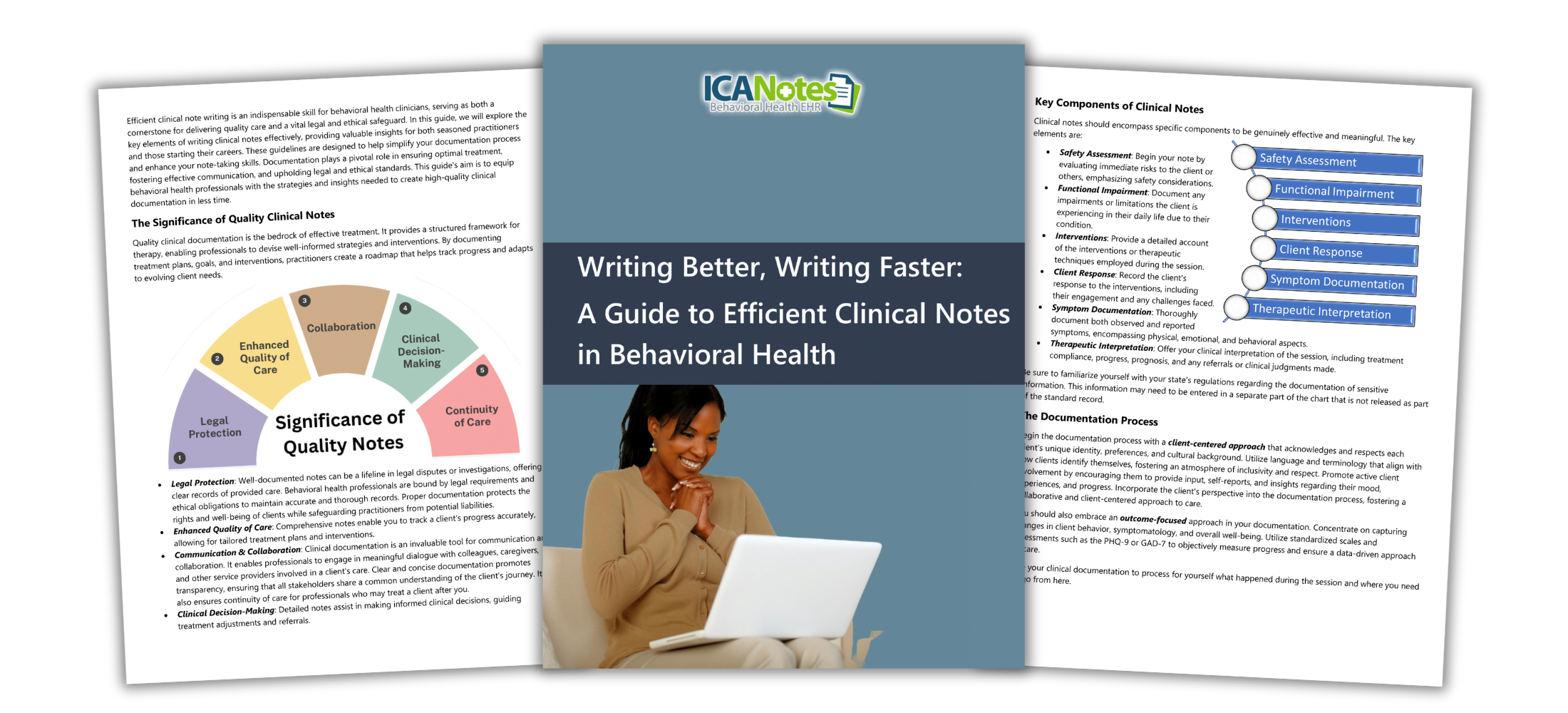
Download our Free Guide to Writing Better Notes
This resource is essential for any clinician looking to save time while maintaining high standards in documentation. This guide covers streamlined note-writing techniques, and best practices for organizing progress notes and treatment plans.
2. You Shouldn't Use the Patient's Words
This myth is quite literally the opposite of what you should be doing. Including a client's words is an essential part of your behavioral therapy clinical notes. In each session, write down at least one verbatim statement from your patient. Quotes might include how they're feeling, their thoughts and what they're seeking help with. Recording the patient's words will give you the most accurate depiction of their condition.
Quotes are beneficial for differentiating your interpretation from something a client legitimately said, which can be crucial in lawsuits and court cases. For example, if a patient or their family chooses to sue you for a misdiagnosis, your notes can help protect you. If you documented direct quotes from the patient in your notes that influenced your judgment, you can help other mental health professionals and a judge understand how you arrived at a specific diagnosis. When psychiatrists include information like quotes in their notes, they win these cases 80% of the time.
Additionally, if the same patient denies their symptoms in front of a judge or other behavioral health professional, your notes containing their quotes will help prove what they claimed to be feeling during your sessions. When your patients tell you how they've been feeling or if something they said stands out to you, write it down — especially if it helps you determine a diagnosis or treatment plan.
3. You Shouldn't Talk About Suicide in the Note
As a mental health professional caring for your patients' well-being, you should be open about discussing suicide in your sessions and in your notes. Some therapists and behavioral health clinicians may worry about documenting their patients' suicidal thoughts or feelings out of fear that they will someday stand accused of doing nothing about it. While these feelings are valid, it's crucial to acknowledge the reality of your clients' situation and what you're doing to help, based on what they've shared with you.
Lawsuits against mental health professionals regarding a patient's suicide are becoming more standard. It's vital to have conversations with your patients about suicide and whether they have any suicidal ideations, their risk factors and what their loved ones' thoughts are. Even if your patient insists they don't have suicidal thoughts, make a note of this. If you end up in court, a judge will want to see that you did everything you could with the information available to you.
Clearly document suicidal assessments to protect yourself and provide better care for your patients.
4. You Shouldn't Record How the Patient Looks
A crucial part of your notes should include observations about your patients' behavior. Doing so can help you determine patterns that will paint a picture of how each client is doing. These observations can include several things, like what the patient is wearing, their hairstyle and color, whether they bring a cup of coffee, if they show excitement or reluctance, etc. Describe how your patient appears and behaves during the session and what your interpretations of this behavior are.
For example, let's say you have a patient who regularly comes to her appointments on time, well-dressed and with her hair and makeup done. For today's session, she was 10 minutes late and came wearing sweatpants, a baggy shirt and her hair looked untouched. Based on the behavioral pattern you've identified in previous session notes, you could infer that your patient isn't feeling like herself today. Note and discuss this, so you can track changes throughout treatment.
What to Include in the Notes
What you include in your mental health notes might vary depending on the type of session it is, your state or practice guidelines for notes and whether you're using a specific template. Regardless, you should always include these three things to make your notes as thorough as possible.
- Observations: Observations can include symptoms your patient tells you about, what you notice about the client, their behavior, observable signs, your interpretations and any objective data or information.
- Assessment: Next, you'll want to include your evaluation of your patient's condition, as well as the intervention techniques or activities you applied during the session. For example, if your client expressed feeling stressed about work, jot down what coping strategies you suggested.
- Treatment plan: Every session note should clearly describe your treatment plan for your patient and their progress — or lack thereof — toward it.
Be sure to include any information that helped you form your diagnosis, plus any other relevant details the client shares.
Avoid These Clinical Notes Myths With ICANotes
ICANotes electronic health record software can help you write thorough notes efficiently for each therapy session. Use our menus of buttons and custom fields to quickly document observations, symptoms, diagnoses and a treatment plan for each patient and session. Use our templates for various psychiatric and therapy notes and assessments to ensure you're documenting everything you need.
To find out how ICANotes can help you write better clinical therapy notes, contact our support team today.