Creating Treatment Plans for PTSD
Post-traumatic stress disorder (PTSD) happens after someone experiences or witnesses a traumatic event, such as domestic violence, war, a terrorist attack, or sexual assault, or it can occur after repeated exposure to horrific experiences. More than half of adults experience PTSD in their lives. PTSD has gone by many names, including shell shock after WWI and combat fatigue following WWII.
Regardless of its name, PTSD manifests in the same way. Common PTSD symptoms include:
- Nightmares
- Traumatic flashbacks
- Fear, anger, and sadness
- Detachment from others
Therapists treating this condition should create treatment plans for PTSD, which should describe patient symptoms, evaluate the best course of action for treatment, establish a timeline to achieve goals, and enact a method for therapists and patients to measure progress. A PTSD treatment plan comes with many benefits, including guiding treatment, reducing fraud by documenting all services, and facilitating potential patient transfers to a new therapist.
Below, we'll discuss what a PTSD treatment plan should include and how to keep solid documentation.
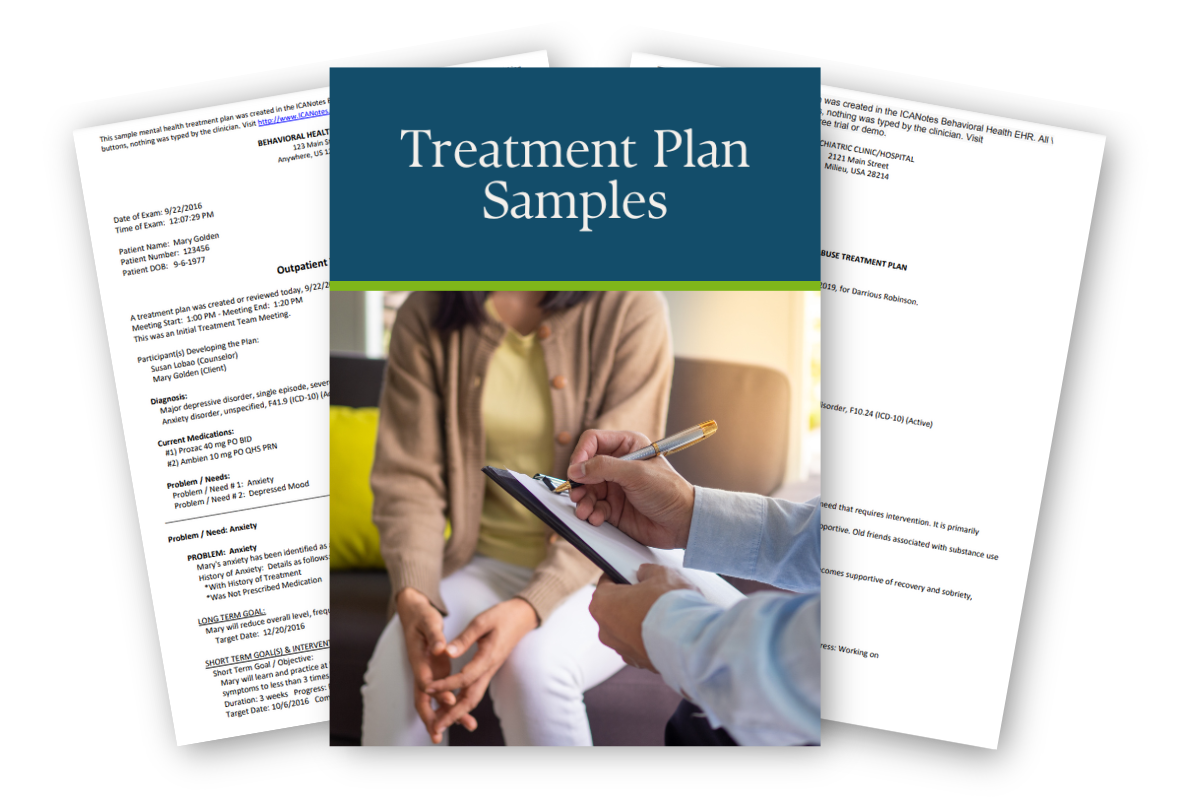
View Our Sample Treatment Plans
Get instant access to our full library of sample treatment plans.
Identify the Cause of PTSD
PTSD has various causes depending on an individual's unique circumstances. Common causes of PTSD include traumatic events like physical or emotional assault, a threat with a weapon, an accident, or exposure to violent combat.
Although PTSD symptoms vary depending on the individual and their situation, they typically adhere to four categories:
- Intrusion: Intrusive thoughts include repeated negative flashbacks, memories, and nightmares. When people experience intrusive thoughts, they might feel like they're reliving a traumatic experience.
- Avoidance: People with PTSD may try to avoid people, situations, places, and objects that remind them of a traumatic event. Part of avoidance could include not wanting to speak about a traumatic event to avoid thinking about what happened.
- Cognition and mood alterations: PTSD can cause people to feel negative and distorted thoughts about themselves, their situation or others. They also could struggle to remember crucial details about the traumatic event. Distorted thinking could lead to someone who has PTSD unnecessarily blaming themselves or others. Common symptoms of alterations in mood and cognition include avoiding activities they previously enjoyed, being unable to experience positive emotions like happiness, feeling emotionally numb or feeling detached from loved ones.
- Changes in emotional arousal or reactivity: When people experience PTSD, they might encounter emotional changes such as reckless or self-destructive behavior, irritability, trouble with sleep or concentration, intense awareness of their surroundings, or easy startling.
After identifying whether a patient has PTSD based on their symptoms, you should determine what's caused it. While the causes of PTSD vary depending on each patient, common aspects that could exacerbate a patient's condition include:
- Extreme or repeated stress
- Early-life trauma such as physical or sexual abuse
- Family history of mental health issues
- Substance abuse issues, such as heavy drinking or drug use
- Lack of a solid support system of loved ones
- The patient's inherent personality features, often referred to as temperament
- Biological factors such as how a patient's brain responds to stressful stimuli and how the body regulates hormones
Set PTSD Treatment Goals and Objectives
The ultimate aim of creating treatment plans for PTSD is to help patients reach their goals while letting counselors monitor progress and make necessary adjustments. Part of crafting a PTSD treatment plan is to help patients set realistic goals and objectives for themselves. Although goals and objectives have similar purposes for patient recovery, they do have slight differences. While goals encompass general statements about what patients would like to achieve, objectives target specific skills patients must develop to reach their goals.
When patients set goals and achieve them through specific objectives, they can experience various benefits, including:
- More progress toward recovery
- Improved concentration and motivation
- Increased ability to set priorities
- Boosted self-confidence
- Fewer feelings of being overwhelmed
You can work with patients to set objectives to achieve their goals. First, talk with patients to help them identify unhealthy behaviors and establish goals. Then, you can help them reach those goals by breaking the process into objectives, which are easily digestible steps to change unproductive behaviors and adopt healthy ones.
Potential goals and their corresponding objectives include:
- Processing and working on abuse or neglect issues: Work with patients to help them review incidences of abuse or neglect. You should create a set number of strategies to cope with stimuli that trigger memories of stressful events.
- Working on anger and mood issues: You should help your patients have a favorable view of their life and future when working on mood and anger issues. Encourage positive self-talk to mitigate depression and help celebrate small achievements. Working with patients to set sleep goals can help stabilize their moods. You should also work with them to decrease suicidal thoughts and encourage them to call hotlines if they're experiencing such thoughts.
- Resolving anxiety: Anxiety often accompanies PTSD. You can help patients achieve their goals of managing anxiety by recognizing anxiety-provoking triggers. Further, patients can develop strategies to help build self-confidence and learn which daily situations stress them out.
- Improving behavioral issues through positive behavior: You can help encourage positive behaviors and moods by monitoring drug and alcohol abuse, discouraging patients from high-risk situations that could provoke anger or encouraging them to successfully complete household tasks.
- Communicating better with others: If your patient struggles with communicating with friends and family after a traumatic event, you could set goals to help them establish positive relationships. Objectives that can help patients better communicate include expressing feelings through words and without acting out, understanding behaviors that could cause relationships to fail, and managing physical aggression.
- Managing alcohol and drug abuse: Substance abuse is a symptom of PTSD. When helping patients achieve the goal of resolving drug and alcohol issues, you can work with them to create a PTSD treatment plan. Encourage them to avoid people or places that could spark temptation, and help them discover their triggers for substance abuse.
Use a PTSD Treatment Plan Template
Treatment plans for PTSD are collaborative between the patient and therapist, and they are individual to the patient. However, you can follow a standard template when crafting a PTSD treatment plan. Typical treatment strategies cover common categories, including:
- Patient information: On patient treatment plans, you should document standard patient information such as their name, date, insurance details, and their Social Security number.
- Diagnosis: Next, you'll want to include information about what a patient is experiencing and what is causing their symptoms to come to a diagnosis.
- Challenges and areas for improvement: In this section, report on the goals you've worked on with patients. At this stage of the treatment process, you should also set a specific objective for patients to achieve their goals. Typically, it would be best if you aimed to have at least three goals at any given time with patients.
- Interventions: Interventions should be specific to the patient, set within a particular time frame and measurable.
- Finalization and signatures: At this stage, the patient and clinician both review and sign the treatment plan in approval.
When crafting a PTSD treatment plan, you should first consider how patient problems align with the six problem domains. The domains include:
- Medical status
- Employment and financial support
- Substance abuse
- Legal status
- Family, economic, demographic, and social status
- Psychiatric status

Set SMART Goals on a PTSD Treatment Plan
You'll want to ensure that patient goals match the problem statements and are attainable. Consider how and when patients will achieve certain aims by helping them set SMART goals. SMART goals adhere to the following guidelines:
- Specific: Patients must be easily able to follow the explicit goals you set. While a patient might set a goal of putting themselves in more social situations, a therapist could help guide them toward the objective of going to a certain number of social gatherings or talking to their friends a certain number of times a week.
- Measurable: Measuring patient progress is crucial for motivating both patients and therapists. Patients can track and document their progress through processes like journaling.
- Attainable: Overly ambitious goals may actually do more harm than good. While a goal may be challenging, patients should still have the resources, time, mindset and abilities to achieve it. If they set unattainable goals, they may feel discouraged or discontinue therapy.
- Relevant: Goals must relate to the patient so they can remain motivated to continue working on their objectives. Even if your patient might not understand how achieving the goal currently relates to them, you can help make the patient central to the objective. For example, if someone struggles with communicating with others, you can encourage them to start a group hobby they enjoy.
- Time-limited: Help patients understand how long their treatment will last by setting a date they can aim for to achieve their goals. You can select dates for patients to reach each milestone, breaking their goals into easily digestible chunks.
When setting SMART goals, keep the patient's current state and progress in mind. Goals should be appropriate for where an individual is in their treatment path.
Decide on a Treatment Type
While most treatments follow the same pathway, you should individualize treatment plans for PTSD for each patient. When considering how to write a PTSD treatment plan, consider how different patients may react to different treatments. You'll be able to individualize a treatment type for patients after identifying the cause of their PTSD and helping them set goals.
Four popular treatment types include cognitive behavioral therapy, cognitive processing therapy, cognitive therapy, and prolonged exposure.
1. Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) aims to help patients improve their functioning by changing thought and behavior patterns. With this type of therapy, therapists help patients identify the relationship between their thoughts and behaviors to impact their entire well-being positively. For example, working with a patient to cope with depression and other negative feelings can help them change negative behaviors like substance abuse.
Typically, this treatment is delivered through 12 to 16 sessions. Therapists can help patients through CBT by working with them to re-evaluate their assumptions and thinking patterns, which are frequently called distortions. Examples of distortions include negative thinking, overgeneralizing, or an expectation of a catastrophic outcome.
Controlled exposure can also help patients with avoidance. Further, therapists can help individuals understand how trauma affects them and teach them relaxation techniques to manage trauma-related stress. After learning how to manage stress, patients will be more self-confident and feel more control over their lives.
2. Cognitive Processing Therapy
Cognitive processing therapy (CPT) helps patients reconceptualize a traumatic event to change unhelpful thought processes. CPT is a type of cognitive behavioral therapy and is typically delivered in 12 sessions. Therapists first educate patients about how PTSD affects thoughts and emotions to help them identify which thoughts exacerbate their symptoms. At this stage, a patient can evaluate their current state by writing a statement about their understanding of the traumatic event and how it's impacting them and others.
Next, patients more directly confront the traumatic event by recounting the worst of the trauma. They do this by writing about the traumatic event and reading it during the next session, helping them deal with avoidance. Therapists should help patients directly target and change negative thinking, eventually using adaptive strategies outside of therapy sessions with out-of-session assignments.
3. Cognitive Therapy
Cognitive therapy (CT) also derives from cognitive behavioral therapy and suggests that a patient's symptoms will worsen if they process traumatic events in an unhealthy way. Often, a patient who negatively processes a traumatic event will experience feelings of constant threat or danger. They develop harmful coping mechanisms and re-experience aspects of the trauma.
Treatment typically takes about three months. While treatment methods are similar to CBT, CT uses treatment strategies in a slightly different way. First, therapists help patients understand the meanings behind their negative thoughts and memories and recognize how negative evaluations of the event may exacerbate current feelings of threat.
Then, therapists work with the patient to re-evaluate and change their feelings by creating a traumatic event narrative. The patient's accounts should begin before the traumatic event occurred and end in a place where the patient feels confident and secure. Controlled exposure through visiting the location where the event occurred or writing a narrative about the trauma can help with cognitive restructuring. Finally, patients implement cognitive restructuring by identifying and changing negative behaviors like thought suppression or rumination.
4. Prolonged Exposure
Avoidance of things that remind patients of a traumatic event is a common symptom of PTSD. Prolonged exposure (PE) can help individuals by gradually enabling them to approach negative feelings, experiences, and situations they associate with the traumatic event. Avoidance enforces feelings of fear. However, PE helps patients realize stimuli that remind them of a traumatic event aren't dangerous and can be confronted rather than avoided.
Treatment typically takes about three months. Like other treatments, therapists first assess a patient's situation and past experiences. Then, patients learn breathing techniques to help with dealing with stressful stimuli. Then, therapists reassure patients that therapy is a safe space to explore frightening experiences that remind them of a traumatic event.
During sessions, patients practice imaginal exposure, where they recount the event in the present tense before discussing how the exercise made them feel. A therapist records the patient during this exercise to replay the patient's account, helping them further process what happened. Outside of therapy sessions, patients work to gradually confront previously discussed triggering stimuli.
Prescribe Medications
Although a common set of medications are typically prescribed to treat PTSD, medical intervention should be specific to each individual. Selective serotonin reuptake inhibitors (SSRIs) are most commonly used for treating PTSD. SSRIs manage the activity of serotonin, a neurotransmitter that affects mood and anxiety disorders, in the brain.
Common SSRIs prescribed for PTSD include:
- Sertraline (Zoloft)
- Paroxetine (Paxil)
- Venlafaxine, a serotonin-norepinephrine reuptake inhibitor (SNRI)
Currently, only sertraline and paroxetine are approved to treat PTSD, but other medications have different levels of evidence that support their effectiveness for treatment. Patients who experience adverse side effects from antidepressants or take other medicines that could interact with SSRIs should be prescribed alternative treatments.
Document PTSD Treatment Plan Progress on Notes
Taking clear, detailed notes is crucial when creating treatment plans for PTSD. Note-writing helps clinicians better treat patients by clearly charting their process. Clear notes are also helpful for both internal and external medical professionals to understand a patient's symptoms and how other healthcare staff have treated the patient.
However, clinicians may face challenges with clinical documentation as the healthcare environment becomes increasingly complex. Common concerns clinical staff have with documentation include:
- Spending too much time on documentation
- Passing healthcare regulations
- Having under-coded notes and rejected claims, leads to lost revenue
- Finding software that integrates with electronic billing and practice management
Electronic health records (EHR) for behavioral health fields can help clinicians prevent and resolve these problems. EHRs allow clinicians to take notes and store documents in an organized way. The best systems streamline practice management with intuitive templates for efficient note-writing, patient portals, teletherapy features, and integrated billing software.
Create a PTSD Treatment Plan for Success
ICANotes is a behavioral health EHR that optimizes the clinical documentation process for efficiency and accuracy. You'll save time writing notes so you can focus on what matters most: your patients. Our EHR will securely store client notes and keep your organization compliant with federal regulations, and you can create treatment plans quickly with minimal typing.
Contact us, start your free trial, or schedule a live demo today to learn how you can improve patient care with an EHR!
Start Your Trial Today