The Importance of Telehealth Parity Laws

The purpose of telehealth services is to allow physicians, clinicians, therapists and other healthcare providers to offer treatment virtually for patients from almost any location. With the importance of social distancing since the start of the COVID-19 pandemic, telehealth has become a valuable tool in giving patients the medical and behavioral health care they need.
In 2021, four in 10 Americans used some form of telehealth service to connect with a medical or mental health professional, which shows how common these services have become since the pandemic. Telehealth parity laws play a huge role in the wide range of telehealth services that medical and behavioral health professionals can offer. These laws make it possible for patients to get equal or comparable access and benefits to health care regardless of whether it relates to their physical or mental conditions.
Table of Contents
- Understanding What Telehealth Parity Means
- Why Telehealth Parity Laws Are Crucial in a Post-COVID-19 World
- States With Telehealth Parity Laws
- How to Know if a Plan Must Follow Parity
- Common Objections to Telehealth Parity
Understanding What Telehealth Parity Means
Mental health parity provides a sense of equality for those seeking medical treatment in the form of telemedicine. However, parity is only effective when healthcare plans and providers abide by its rules to uphold its purpose. The Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 laid down the legislation for parity and generally prevents health insurance plans or insurance providers from placing limitations on benefits for those with a mental health or substance use disorder.
This law ensures that large group mental health plans cannot impose less than favorable annual or lifetime dollar limits on benefits comparable to medical and surgical procedures, helping create parity between the two sectors of health. Before the MHPAEA, mental health and addiction treatment usually had far less coverage in health insurance policies than physical illnesses.
Telehealth parity is generally similar to these laws. If a patient has an insurance plan with parity that would grant them unlimited medical visits in person, they have the right to equal treatment and care for their condition through telemedicine and telehealth. The Medicare Telehealth Parity Act of 2017 expanded telehealth coverage to include more services under Medicare.
This means a patient would have as much access to unlimited telehealth visits for their diabetes or heart disease as they would for in-office appointments. Essentially, in states with telemedicine parity laws, your patient would be reimbursed for telemedicine services just as they would be reimbursed for in-person treatment.
It's important to note that while parity provides many with the opportunity for virtual treatment that equals the limits and benefits of their in-person medical care, it doesn't necessarily mean the coverage will be particularly good. A patient's health insurance plan or policy can still limit their coverage even in states with strong parity laws just as coverage varies with health insurance for in-person visits.
Why Telehealth Parity Laws Are Crucial in a Post-COVID-19 World
The COVID-19 pandemic facilitated the use of virtual technology for millions of people to work from home and limit the spread of infection. A positive aspect of this widespread use of technology is the support of telemedicine. The Centers for Medicare and Medicaid Services (CMS) recently added 85 covered telehealth services under Medicare, ensuring patients with plans under parity laws will receive the same reimbursement rate as in-person visits.
When combined with telehealth parity laws, telehealth services widen the margin of accessibility for patients to receive valuable medical care for physical or mental illness while safely quarantining from their homes. This convenience alone helps limit the risk of exposure to others, including healthcare providers who are the most critical weapon in fighting the pandemic.
Without access to telehealth, many people may refuse to seek medical treatment in person for fear of contracting COVID-19. This decision can lead to patients delaying their care until it gets worse and becomes an emergency, which only places additional stress on hospital and emergency departments that are already overrun.
In this case, it's important for states to adopt temporary telehealth parity laws to cover the needs of patients and improve public health through the COVID-19 pandemic and future pandemics that could arise. However, telehealth visits should not replace in-person visits with healthcare providers. Telehealth services are appropriate for common, minor medical conditions or concerns, whereas doctors and counselors must treat severe or chronic physical or mental illnesses in person.
For example, telehealth parity laws should apply in specific conditions unrelated to the pandemic only when the telehealth visit would offer the same value as an in-person visit, otherwise, the treatment would not be comparable.
While there are certain aspects to consider with telehealth services, especially when trying to limit person-to-person contact, telehealth parity laws must be in place to ensure everyone's safety. The widespread use of telehealth during the pandemic also provides the public and legislators with necessary information and data about telehealth use and how they can improve it in the future.
States With Telehealth Parity Laws
Just as with many laws, parity laws differ according to various health insurance plans and certain limitations in some states. Federal parity laws make some inclusion of benefits optional, so conditions and policies vary from state to state depending on the type of treatment and coverage required. For example, if a specific state has strong parity laws, then its regulated health insurance plans must abide by those laws.
These telehealth laws require commercial insurers to cover telehealth, but not all laws require them to pay for telehealth and in-person services at equal reimbursement rates. Only a few states have payment parity laws, but the pandemic has influenced telehealth legislation and regulation in terms of Medicaid reimbursement. While all 50 states and the District of Columbia have some degree of Medicaid reimbursement for their public telehealth programs, the extent of the reimbursement varies.
Telehealth and telemedicine are often used interchangeably and have been slowly expanding even before the pandemic. According to the American Telemedicine Association, 40 states have implemented policies to expand their telemedicine coverage and reimbursement since 2017, which also highlights the value of these services and how critical they are to so many patients.
Still, the pandemic continues to largely impact other aspects of state telehealth and telemedicine parity laws, and this number could grow as the pandemic continues to have a detrimental impact on healthcare workers. For instance, 36 states allowed telehealth services in 2019. As of May 2020, that number jumped to 51, including all 50 states and the District of Columbia. These policy changes after the pandemic also generated an increase in telehealth for similar services including dental care, behavioral health, physical therapy and maternity.
These growing numbers reflect the importance of telehealth parity laws in the case of public health emergencies, ensuring that patients receive the care they need under parity coverage without increasing the spread of illness. Medicare telehealth policies have rapidly changed and updated throughout the pandemic and — most likely — will continue to do so as legislators gain new information and enact plans accordingly.
How to Know if a Plan Must Follow Parity
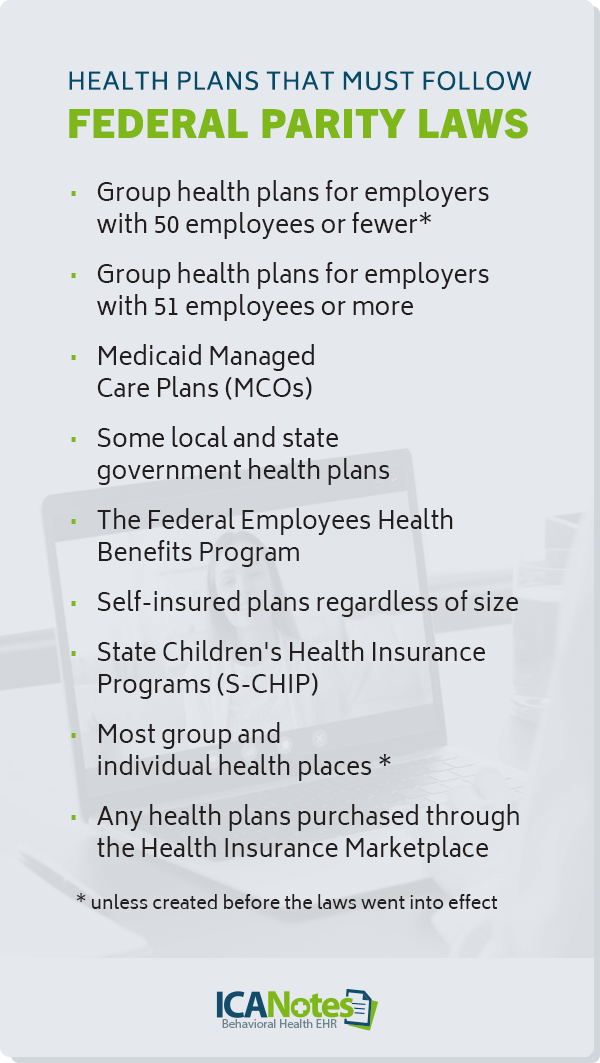
While the MHPAEA provides certain protections on coverage, a federal parity law may only cover a patient's plan depending on the health plan they have and the limits within it. Here are health plans that must follow federal parity laws:
- Group health plans for employers with 50 employees or fewer — unless created before the laws went into effect
- Group health plans for employers with at least 51 employees or more
- Medicaid Managed Care Plans (MCOs)
- Some local and state government health plans
- The Federal Employees Health Benefits Program
- Self-insured plans regardless of size
- State Children's Health Insurance Programs (S-CHIP)
- Most group and individual health places — unless created before parity laws went into effect
- Any health plans purchased through the Health Insurance Marketplace
Common Objections to Telehealth Parity
Health insurance plans are not created equal, even with the help of parity laws, when it comes to mental health and substance abuse treatment. With the rise of telehealth and telemedicine, some specific challenges raise objections among healthcare workers — especially when it comes to reimbursement.
Reliability and Quality Care
A common argument against telehealth parity is that many consider the services to have less value than in-person care — making them less effective or reliable. However, low-value care can exist in in-person settings depending on the provider, not the mode of delivery. For certain illnesses or conditions, a physical examination would allow the physician to provide a more in-depth analysis of symptoms for physical or mental conditions. But it doesn't mean that telehealth cannot provide the same quality care.
For example, during the start of the pandemic, over 65% of patient visits were conducted virtually, with over 31% of those patients opting for telephone care. Minimizing or eliminating payment for audio-only telehealth services excludes many patients who live in rural areas without any internet or digital access. These patients — especially during a widespread pandemic — might lose the option for reliable medical care completely if they were not able to visit an in-person facility.
Clinical Effort
Plenty of factors influence the amount of clinical effort physicians and clinicians give to their patients, but telehealth is not one of them. According to the American Medical Association, these are the top four factors that define clinical effort:
- The complexity of a patient's diagnosis
- The time spent in patient's care
- The risk of management options
- The volume of data reviewed
These factors are also considered independent from mode of delivery and used to determine reimbursement for various clinical visits. According to the same AMA document on evaluation and management coding, clinicians are not required to perform and document a physical exam unless necessary when choosing billing levels. So, while it may be plausible to assume that telehealth requires less effort because it is not conducted in person — and while physical exams are essential for some diagnoses and treatments — clinical effort is otherwise comparable in both instances.
In addition, therapists and counselors can perform the majority of behavioral health services, which often rely heavily on communication, without needing to see patients in person. Online therapy has skyrocketed since the pandemic, and many predict it to stay because of the flexibility benefits. Many behavioral healthcare workers are advocating for continued use with the help of HIPAA-compliant platforms to expand these services.
Overuse
Another concern about telehealth parity laws is that they will lead to overuse, abuse or fraud. While it's noteworthy to mention telehealth use is 20 times higher than it was before the pandemic, the total weekly visits have not exceeded those before the pandemic. This means that telehealth has only become a substitute for in-person care as it has become necessary, but it's not entirely taking over in-person visits.
Cost-Savings
In addition to the perceived low quality of care, some argue that telehealth costs less to deliver than in-person care. While it might cost less up-front to use telehealth compared to in-person care, telehealth reaches a wide range of patients who may have otherwise not been able to access medical or mental health care, which could increase a practice's patient base.
But that doesn't always mean that telehealth drastically reduces a practice's expenses. CMS establishes payment rates for patient visits based on the general costs of clinical effort, malpractice insurance and practice expenses — and these expenses do not differ much between in-person and telehealth outpatient visits.
The costs saved by reducing the supplies needed for in-person medical or behavioral health care help offset the expenses to install and maintain telehealth services and teach staff and patients how to use them.
While some believe that telemedicine should not be reimbursed on an equal level to in-person care, the loss of revenue associated with low reimbursement may not make telehealth worth it for many practices, excluding the patients who truly benefit from it.
Patient Privacy
Some patients and physicians who are new to telehealth are concerned about patient privacy as medical records and information become digitized. This concern relies on the idea that digital records are more vulnerable to hacking or inappropriate use, which only presents a risk when a practice uses a system or platform that is not secure.
Some telehealth platforms might also put the responsibility of communicating appointments and results on the patient rather than the healthcare professional, making it more challenging to reap the benefits of convenience that telehealth brings.
Implement Secure Telehealth Services With ICANotes
Telehealth parity laws are essential for allowing patients to have multiple means of accessing health care for a myriad of services. While challenges and considerations of healthcare providers toward telehealth are valid during certain circumstances, it's clear that the benefits outweigh those considerations — particularly during a pandemic. Your practice and patients can benefit from enhanced telehealth services with ICANotes, a clinically robust EHR feature with a HIPAA-compliant video conferencing platform.
We know how important it is for your patients and clients to receive care in a time when health organizations encourage social distancing whenever possible. ICANotes offers the telehealth solution that removes barriers, improves convenience and reduces the social stigma of telehealth services. Start your free trial today or schedule a live demo to experience our fully integrated platform for scheduling, patient portals, appointment reminders and other features.
Sources
- https://www.psychiatry.org/newsroom/news-releases/New-Nationwide-Poll-Shows-an-Increased-Popularity-for-Telehealth-Services
- https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/mhpaea_factsheet
- https://www.apa.org/topics/managed-care-insurance/parity-employers
- https://www.congress.gov/bill/115th-congress/house-bill/2550/text
- https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7462835/
- https://www.americantelemed.org/in-the-news/telehealth-policy-and-reimbursement-vary-widely-from-state-to-state-ata-report-finds/
- https://www.cchpca.org/topic/parity/
- https://track.govhawk.com/reports/24PKO/public
- https://www.cchpca.org/resources/state-telehealth-laws-and-reimbursement-policies-report-fall-2021/
- https://www.americantelemed.org/in-the-news/ata-40-states-have-expanded-telemedicine-coverage-reimbursement-since-2017/
- https://aspe.hhs.gov/sites/default/files/2021-07/medicaid-telehealth-brief.pdf
- https://www.cchpca.org/resources/covid-19-telehealth-coverage-policies/
- https://www.nami.org/Your-Journey/Individuals-with-Mental-Illness/Understanding-Health-Insurance/What-is-Mental-Health-Parity
- https://www.ajmc.com/view/differences-in-the-use-of-telephone-and-video-telemedicine-visits-during-the-covid-19-pandemic
- https://www.aapc.com/evaluation-management/em-codes-changes-2021.aspx#2021CPTEMGuidelinesforMDM
- https://www.apa.org/monitor/2021/01/trends-online-therapy
- https://www.healthaffairs.org/do/10.1377/forefront.20210503.625394/full/
- https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2022-medicare-physician-fee-schedule-final-rule
Free Ebook: Going Virtual
Everything you need to start a virtual behavioral health practice.