Blog > Documentation > How to Write Mental Health Progress Notes: Tips, Templates & Examples
How to Write Mental Health Progress Notes + Examples and Templates
Writing mental health progress notes is part of every session, but it can feel overwhelming. You need to stay compliant, support medical necessity, and keep notes clear and focused. This guide shows you what to include, how to choose the right format, and how to write progress notes that are fast, accurate, and clinically effective. You’ll get examples, ready-to-use templates, and tips to help you spend less time documenting and more time with your clients.

Last Updated: December 19, 2025


What You'll Learn
-
What mental health progress notes are — and why accurate, compliant documentation matters for care continuity and reimbursement
-
How to write progress notes using clear, clinically appropriate language that supports medical necessity
-
The key components every high-quality progress note should include, regardless of note format
-
Common progress note formats (SOAP, DAP, BIRP) and when to use each in clinical practice
-
Step-by-step guidance on structuring progress notes that meet payer, audit, and compliance expectations
-
Real-world progress note examples and progress note samples you can reference or adapt
-
Documentation tips to avoid vague, duplicative, or audit-risk language in progress notes
-
How progress note templates and EHR tools can streamline documentation without sacrificing clinical quality
Contents
- What are Mental Health Progress Notes?
- Purpose of Progress Notes
- What Should be Included in Mental Health Progress Notes?
- Popular Mental Health Progress Note Templates with Examples
- Examples of What to Include in a Progress Note Template
- Sample Progress Notes
- Practical Tips for Writing Better Mental Health Progress Notes
- How to Bill and Code Progress Notes
- Why You Should Use EHR Software for Progress Notes
- FAQs: Mental Health Progress Notes
- How ICANotes Helps Clinicians Write Better Mental Health Progress Notes
What Are Mental Health Progress Notes?
Mental health progress notes are essential clinical documents written after each session to record the patient's status, symptoms, interventions, and progress toward treatment goals. They help you capture what happened in the session, evaluate the client’s progress, and outline your plan moving forward. These notes serve important purposes across clinical, legal, and billing needs.
Progress notes are not the same as psychotherapy notes. Progress notes are part of the medical record and are often required for insurance claims and compliance. Psychotherapy notes are kept separately, contain personal reflections, and are not typically shared or required for billing.
Unlike casual observations or reminders, progress notes must be:
-
Objective: Focused on observable behavior and clinical facts.
-
Specific: Tied to treatment goals and interventions used.
-
Timely: Written shortly after the session to ensure accuracy.
Related: Psychotherapy Notes vs Progress Notes - What are the Key Differences?
Purpose of Progress Notes
Well-written progress notes serve multiple purposes, including:
-
Tracking patient progress over time.
-
Supporting continuity of care between providers.
-
Establishing medical necessity for services billed to insurance.
-
Creating a legal record in the event of audits or disputes.
-
Facilitating collaboration across multidisciplinary teams.
Clinicians who document consistently and thoroughly not only improve care but also protect themselves against liability and reimbursement issues.
What Should be Included in Mental Health Progress Notes?
A strong progress note for mental health gives a clear, accurate picture of each session. It supports quality care, protects you legally, and helps ensure reimbursement. Every note should include the following core elements.
1. Session Details
Begin with basic session data. These details confirm when and how the session occurred and who was involved. Include:
- Date of service
- Start and end time
- Session format (telehealth or in-person)
- Client’s location if the session was remote
- Client’s name and a second unique identifier (such as date of birth or client ID)
- Provider’s name and credentials
2. Person-Centered Details
Use the client’s own words to describe how they’re feeling or what they’re experiencing. This helps show that the session was specific to their current needs. Focus on statements related to symptoms, stressors, goals, or treatment.
Example: “I’ve been trying to stay calm, but every time my boss calls me in, I feel like I’m about to cry.”
3. Clinical Observations
Document how the client presented in the session. Use objective language to describe what you saw and heard. These observations support your clinical judgment and can include:
- Mood and affect
- Behavior and speech
- Appearance and hygiene
- Eye contact or posture
- Thought content and reasoning
- Level of insight or judgment.
Include at least three elements from the mental status exam to meet documentation standards.
4. Progress Toward Goals
Comment on how the client is moving in relation to their treatment goals. Did they show improvement, decline, or stay the same? Be specific and tie your notes to the treatment plan. If goals have shifted, note that and describe why. This section is essential for showing clinical progress and medical necessity.
5. Risk Assessment
Every note should include a risk statement. If the client expresses suicidal or homicidal thoughts or if there is another concern related to safety, document the risk level and any steps taken. If there is no risk, document that clearly.
Example: “Client denied suicidal and homicidal ideation. No current safety concerns noted.”
6. Plan for Care and Interventions
Describe what you did during the session and what comes next. Include any clinical approach used, such as cognitive behavioral therapy, EMDR, or motivational interviewing. If you assigned homework, reviewed coping skills, or made a referral, include that as well. This section shows your clinical reasoning and outlines the direction of treatment.
Example: “Reviewed grounding techniques. Assigned journaling exercise. Next session scheduled for Tuesday.”
Download Our Guide to Writing Better, Faster Clinical Notes
Streamline your progress notes, avoid documentation pitfalls, and stay compliant with practical templates, note formats (SOAP, DAP, BIRP), and time-saving tips to write high-quality, defensible notes faster.
Popular Mental Health Progress Note Templates with Examples
There are several standardized formats clinicians can use when writing progress notes, including SOAP, DAP, and BIRP. Each format organizes clinical information differently, but they all aim to capture the same essential components: client presentation, interventions used, clinical assessment, and the treatment plan moving forward.
The best format often depends on your clinical setting, documentation requirements, and personal preference. What matters most is consistency, clarity, and compliance with standards for medical necessity and continuity of care.
Here are the most common formats with examples.
1. SOAP Notes
Subjective, Objective, Assessment, Plan
The SOAP note format is common across healthcare settings. It breaks each note into four sections, helping you separate client input from your observations and clinical judgment.
Subjective: The client’s self-reported symptoms, concerns, goals, and stressors. Use their exact words when possible.
Objective: Your professional observations. This includes the client’s appearance, behavior, affect, and other measurable data.
Assessment: Your interpretation of the client’s condition, progress, or setbacks, based on both subjective and objective information.
Plan: What happens next? This includes your interventions, planned treatment strategies, follow-ups, and homework.
2. BIRP Notes
Behavior, Intervention, Response, Plan
The BIRP note format focuses on what happened in the session and how the client responded. It’s ideal when you want to emphasize real-time interaction and behavior change.
Behavior: What the client shared and how they presented in the session. Include both verbal and nonverbal behavior.
Intervention: The techniques or strategies you used during the session.
Response: How the client reacted to your interventions. Include engagement, insight, or resistance.
Plan: What you plan to do in the next session, any changes to treatment, and client assignments.
2. DAP Notes
Data, Assessment, Plan
The DAP note combines client input and your observations into a streamlined format. This format works well for therapists who prefer a more narrative style but still want a clear structure.
Data: A combination of what the client reported and what you observed. Focus on current symptoms, stressors, and session focus.
Assessment: Your clinical interpretation of what’s going on. Include symptom patterns, risk, progress toward goals, and diagnosis-related insight.
Plan: Outline what happens next. Note interventions, homework, follow-up steps, or referrals.
Examples of What to Include in a Mental Health Progress Note Template
Though we briefly mentioned the general structure of progress notes above, let's look at more specific progress note examples and what therapists and other behavioral health professionals must document.
Mental health progress notes provide a clear, clinical record that allows behavioral health professionals to document findings, interventions, and treatment plans using objective medical facts. The required elements of a progress note can vary depending on factors such as payer requirements, state regulations, licensing board guidelines, or your practice setting. To ensure your documentation is both compliant and defensible, it’s essential to verify that your chosen note format and templates align with the standards set by these governing bodies.
In general, all progress notes should include a variation of the following:
-
Date of Session and Start/End Times
-
Client Name or ID
-
Presenting Concern: Summarize the primary issue or focus of the session, as reported by the client or observed by the clinician. This could include symptoms, events, stressors, or goals discussed. Use client language when appropriate (e.g., “feeling overwhelmed at work”).
-
Mental Status/Observations: Describe the client’s appearance, behavior, mood, affect, speech, thought content, orientation, and any other relevant mental status indicators observed during the session. Note any changes from prior sessions or safety concerns.
-
Intervention(s) Used: List the therapeutic techniques, interventions, or modalities applied in the session (e.g., cognitive restructuring, mindfulness, supportive listening, safety planning). Be specific enough to demonstrate the medical necessity of the session.
-
Client Response: Document how the client responded to the interventions — emotionally, cognitively, or behaviorally. Include insights gained, level of engagement, or resistance encountered. Use brief quotes if helpful.
-
Clinician Assessment: Provide a clinical interpretation of the client’s current status and session progress. This may include diagnostic impressions, risk assessment updates, and evaluation of treatment progress. Keep this section objective and grounded in observable behavior or clinical tools.
- Link to Treatment Plan: Reference specific goals or objectives from the client’s treatment plan to show how the session content supports ongoing care. For example, note progress toward a goal (e.g., "Client continues to build coping strategies for managing social anxiety, aligning with Objective 2 in the treatment plan") or update the plan if new concerns arise. This strengthens documentation of medical necessity and demonstrates goal-directed therapy.
-
Plan for Next Session: Outline the next steps in treatment, including follow-up topics, interventions to continue or modify, homework assignments, referrals, or changes in frequency. This helps maintain continuity of care and treatment plan alignment.
-
Clinician Signature and Credentials
You can adapt this progress note template to suit your specific clinical approach, practice requirements, or EHR format.
Progress notes should reflect objective, clinically justifiable information — not personal opinions, assumptions, or unsupported judgments. Focus on what you directly observed and what was discussed during the session. Avoid including content that can’t be validated through clinical evidence or professional assessment. Exceptions may apply if the client discloses a critical incident, major life change, or any risk of harm to themselves or others, these should always be clearly documented.
Sample Progress Notes
Here are two examples of progress notes that demonstrate effective clinical documentation:
Sample Progress Note – Individual Therapy
Client reported increased anxiety related to an upcoming job interview. Used role-play to rehearse responses to common questions and cognitive restructuring to challenge negative self-talk. Client engaged actively and demonstrated improved confidence. Plan to review interview experience next session and introduce exposure hierarchy for social anxiety.
Sample Progress Note – Medication Management
Client reports decreased depressive symptoms on current dose of sertraline 50mg. No adverse side effects noted. PHQ-9 score decreased from 14 to 8. Will maintain current dosage and re-evaluate in four weeks.
These sample progress notes show how to be concise, objective, and clinically relevant.
Sample Progress Note
Date of Session and Start/End Times:
August 27, 2025 | 2:00 PM – 2:50 PM
Client Name or ID:
J.S. (Client ID #74839)
Presenting Concern:
Client reported ongoing stress and anxiety related to an upcoming family gathering, stating, “I’m already feeling tense just thinking about being around them.” She described difficulty sleeping and feeling easily agitated during the week. Identified goal: reduce physiological and emotional reactivity to triggering interpersonal situations.
Mental Status/Observations:
Client appeared well-groomed, alert, and oriented to person, place, and time. Speech was normal in rate and volume. Affect was congruent with stated mood (“anxious and frustrated”). Thought processes were logical and goal-directed. No suicidal or homicidal ideation reported. No psychotic symptoms observed.
Intervention(s) Used:
Provided psychoeducation on the fight-or-flight response and introduced diaphragmatic breathing as a grounding strategy. Engaged client in guided breathing exercise during session. Utilized cognitive restructuring to challenge anticipatory thoughts related to the upcoming event. Reviewed prior use of emotion regulation skills.
Client Response:
Client engaged well in session and reported the breathing technique helped her “feel a little more in control.” She was able to identify distorted thoughts such as “They’re going to judge everything I say” and collaboratively reframe them. Client appeared calmer at the end of the session and expressed willingness to practice new strategies at home.
Clinician Assessment:
Client continues to experience moderate anxiety with identifiable triggers. No risk concerns at this time. Presentation consistent with Generalized Anxiety Disorder (F41.1). Client is demonstrating increased insight and improved ability to apply emotion regulation techniques with clinician support.
Link to Treatment Plan:
Session content supports Objective 2 in the treatment plan: “Develop and apply at least two coping strategies to manage anxiety in social situations.” Client showed progress toward this goal by practicing and responding positively to diaphragmatic breathing and cognitive reframing.
Plan for Next Session:
Review client’s experience implementing breathing and thought-challenging techniques during the family gathering. Introduce visualization strategies if appropriate. Continue building emotion regulation skill set. No change to session frequency at this time.
Clinician Signature and Credentials:
L. Martinez, LCSW
Access Our Sample Notes Library
Get instant access to our full library of sample behavioral health notes, including Initial Evaluations, Progress Notes, Treatment Plans, and Discharge Summaries. We have note samples for psychiatry, therapy, case management, PRP, substance abuse, group therapy, couples therapy, and more!
Practical Tips for Writing Better Mental Health Progress Notes
Clinicians spend an average of 13.5 hours per week on documentation. Reducing that burden with better systems and habits can give you back valuable time for client care. These tips help you document accurately, protect your license, support billing, and save time.
Write Notes Within 24 Hours
Details fade quickly. Writing your note the same day helps you capture important quotes, behaviors, and insights while they are still fresh in your mind. This also supports clinical accuracy and keeps your documentation up to date for audits or supervision.
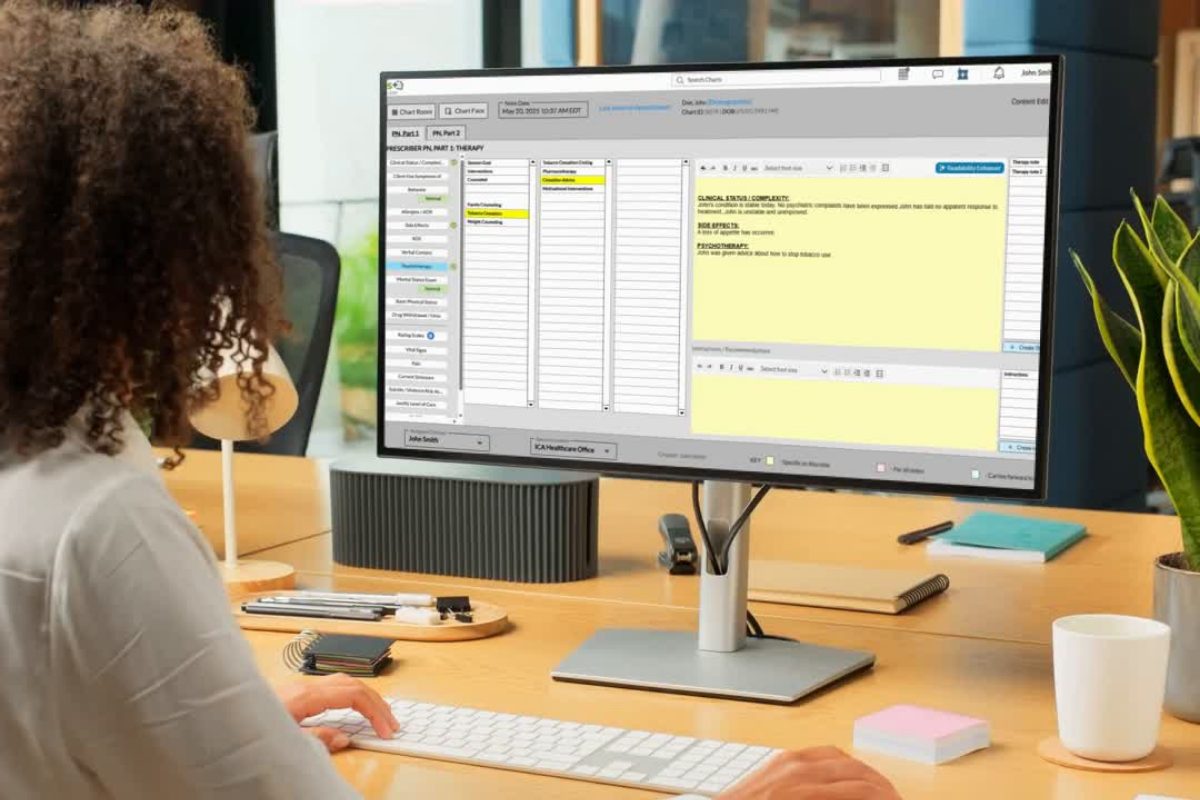
Use ICANotes or a Structured Template
Templates help you stay focused and cover all the required elements. ICANotes provides built-in SOAP, DAP, and BIRP templates with prewritten content, dropdowns, and one-click insertions. This makes it easier to stay compliant and complete notes faster without missing critical information.
Be Objective
Use clear and observable language. Instead of saying "client seemed anxious," describe what you actually saw. For example, "client avoided eye contact, tapped foot repeatedly, and spoke in a quiet tone." This strengthens the clinical value of your note and reduces ambiguity.
Avoid Copy-Paste Traps
Repeating old content can make it look like the client is not making progress. Each note should reflect what actually happened in that specific session. If you’re addressing the same issues, summarize them in a way that shows new insight or different client responses.
Include Direct Quotes
Quoting your client can add context, make your notes more personal, and demonstrate that you are actively listening. Payers also look for this as a sign of individualized care.
Example: "I feel like I’m stuck in the same cycle and don’t know how to break it."
Link Progress to Treatment Goals
Notes should clearly show how the session supported the client’s goals or treatment plan. Mention which goal was addressed, what progress was made, or if there was a need to update the plan. This ties your clinical work to medical necessity and helps justify services.
Document Your Modality
Mention the therapeutic techniques you used, such as CBT, DBT, or EMDR. You can include a sentence like, "Therapist used CBT techniques to challenge negative thought patterns." This helps clarify your clinical reasoning and supports insurance claims.
Always Include a Risk Assessment
Risk must be addressed in every session. Even if there is no concern, document that you checked. A simple line like "client denied suicidal or homicidal ideation and showed no signs of current risk" provides important legal and clinical protection.
How to Bill and Code Progress Notes
Accurate billing starts with strong documentation. Your progress notes must support the time spent, service provided, and clinical reason for treatment. Insurance companies often review notes to ensure the session length and content match the CPT code used.
Common CPT Codes for Behavioral Health
- 90834 — 45-minute psychotherapy session (total time: 38 to 52 minutes)
- 90837 — 60-minute psychotherapy session (total time: 53 to 60 minutes)
- 99204 — 45-minute psychiatric diagnostic intake (typically used by prescribers)
- 99205 — 60-minute psychiatric diagnostic intake (for new patients with complex needs)
These codes must be backed by notes that clearly show what happened during the session and why that amount of time was clinically appropriate.
Your note should clearly justify:
Session length: Include exact start and stop times. This confirms the session duration and aligns with time-based codes.
Clinical necessity: Show why the client needed care that day. Link symptoms or functional impairments to the goals in the treatment plan.
Modality used: Mention the therapeutic approach (for example, CBT, EMDR, MI) to show evidence-based treatment.
How care addressed the diagnosis: Your note should reflect that the session focused on reducing symptoms, improving function, or supporting recovery related to the client’s diagnosis.
Example: “Used CBT to challenge automatic thoughts contributing to depressive symptoms. Client engaged well and demonstrated new insight into behavior patterns.”
This type of documentation helps protect your billing, supports medical necessity, and ensures you get paid for the care you deliver.
Why You Should Use EHR Software for Progress Notes
Depending on how many patients you see and how frequently, you can end up spending several hours every day writing your progress notes. Not to mention, handwritten paper progress notes can present many issues, such as getting lost or damaged. Paper progress notes will also take you much longer to complete than electronic notes.
Research shows that clinical documentation contributes heavily to staff burnout because it takes significant time that therapists and other mental health professionals could instead spend with patients. One study found that clinicians welcome a serious redesign of documentation processes to restore autonomy, eliminate the number of actions that do not add value and return time to staff for more essential care activities.
By introducing EHR software, you can lift the burden of documentation with these benefits:
- Making your notes legible, easy and quick to read
- Reducing documentation errors or missing information
- Preventing lost revenue due to under-coded notes or claims being rejected
- Reducing time spent on documentation and record-keeping
- Leveraging clinical progress note templates for consistency
- Increasing your peace of mind that your notes will comply with regulations and pass an audit.
Progress note software built into your electronic health record (EHR) system can drastically reduce documentation time and improve compliance. Key features to look for in EHR progress note tools include:
-
Auto-populated session details
-
Prebuilt templates for various visit types
-
Click-to-add clinical interventions
-
Built-in risk assessments and outcome measures
-
HIPAA-compliant cloud storage
By reducing manual entry and repetitive tasks, progress note software helps you focus more on clinical care and less on paperwork.
Frequently Asked Questions: Mental Health Progress Notes
How ICANotes Helps Clinicians Write Better Mental Health Progress Notes
Writing effective progress notes can be time-consuming. Without the right tools, providers risk incomplete records, billing delays, and compliance issues.
ICANotes is a behavioral health EHR platform purpose-built to make writing mental health progress notes fast, accurate, and compliant. Our intelligent charting features include:
-
Specialty-specific templates for mental health documentation
-
Structured, menu-driven charting that reduces typing
-
Built-in compliance tools that support medical necessity
-
Group therapy notes that auto-populate across charts
-
EHR-integrated billing, scheduling, e-prescribing, and telehealth to streamline workflow
With ICANotes, you can spend less time writing and more time treating. Whether you’re documenting for therapy, psychiatry, or medication management, our progress note software adapts to your workflow and helps you stay on top of every session.
Ready to streamline your mental health progress notes?
Start your free trial or book a demo to see how ICANotes makes writing progress notes faster and easier.
Start Your 30-Day Free Trial
Experience the most intuitive, clinically robust EHR designed for behavioral health professionals, built to streamline documentation, improve compliance, and enhance patient care.
- Complete Notes in Minutes - Purpose-built for behavioral health charting
- Always Audit-Ready – Structured documentation that meets payer requirements
- Keep Your Schedule Full – Automated reminders reduce costly no-shows
- Engage Clients Seamlessly – Secure portal for forms, messages, and payments
- HIPAA-Compliant Telehealth built into your workflow
Complete Notes in Minutes – Purpose-built for behavioral health charting
Always Audit-Ready – Structured documentation that meets payer requirements
Keep Your Schedule Full – Automated reminders reduce costly no-shows
Engage Clients Seamlessly – Secure portal for forms, messages, and payments
HIPAA-Compliant Telehealth built into your workflow
Related Posts
Dr. October Boyles is a behavioral health expert and clinical leader with extensive expertise in nursing, compliance, and healthcare operations. With a Doctor of Nursing Practice (DNP) and advanced degrees in nursing, she specializes in evidence-based practices, EHR optimization, and improving outcomes in behavioral health settings. Dr. Boyles is passionate about empowering clinicians with the tools and strategies needed to deliver high-quality, patient-centered care.