Exploring Transcranial Magnetic Stimulation (TMS) Therapy for Treatment-Resistant Disorders
If you're a clinician or mental health professional, you understand the challenges of treatment-resistant depression, anxiety and other mental health conditions. While some patients find success with a combination of medications and talk therapy, others have trouble managing symptoms and improving their well-being. Transcranial magnetic stimulation (TMS) therapy can be a game changer for these patients. The minimally invasive, FDA-approved treatment may offer relief for your patients after just a few short sessions.
The following guide will explore how TMS works, its uses and potential advantages and drawbacks.
What Is Transcranial Magnetic Stimulation and Therapy?
Transcranial magnetic stimulation is an FDA-approved, noninvasive form of brain stimulation in which a device applies powerful, repeated magnetic fields to specific areas of the brain. The devices operate outside of the body, impacting central nervous system activity involved in mental health conditions like depression, anxiety and obsessive-compulsive disorder (OCD).
Compared to side effects often seen with medications and electric convulsive therapy (ECT), TMS is generally well-tolerated and does not require anesthesia. The treatment is often recommended when conventional treatments are ineffective or cause unwanted side effects in patients.
TMS was introduced by English medical physicist Anthony Barker in 1985 as a tool for neuropsychology before its therapeutic uses in treating psychiatric disorders. Today, the FDA has approved TMS for treatment-resistant depression, obsessive-compulsive disorder, smoking cessation and migraines. Further research is being conducted on the use of TMS for disorders like epilepsy, pediatric depression and movement disorders.
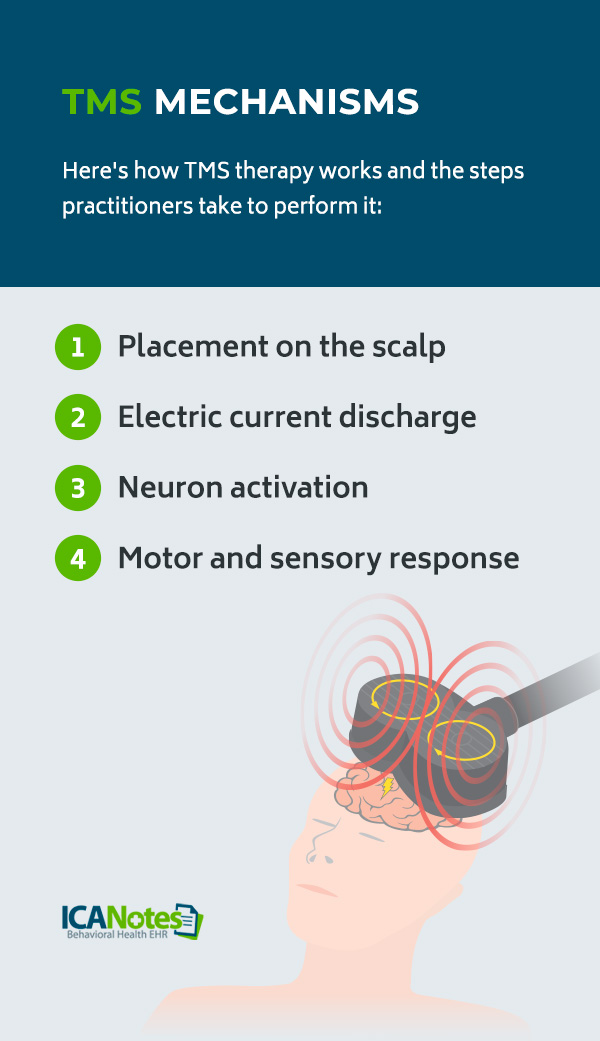
TMS Mechanisms
Here's how TMS therapy works and the steps practitioners take to perform it:
- Placement on the scalp: First, an insulated coil wire, typically encased in plastic, is placed on the patient's head.
- Electric current discharge: An electric current briefly discharges through the coil, producing a weak magnetic field capable of penetrating cranial tissue. The technician can adjust the device to deliver high- or low-frequency pulses.
- Neuron activation: The magnetic field activates neurons in the brain, reaching 0.8 to 1.2 inches beneath the scalp. The actual depth will depend on the magnetic field's rate of change and the current's strength discharged through the coil.
- Motor and sensory response: TMS can induce various motor and sensory responses depending on where it is placed. For example, when placed over the motor cortex or the region that controls movement, the subject's arm, hand or leg may move.
When placed over cells within the brain thought to release neurotransmitters — like serotonin and dopamine involved in depression — TMS is believed to restore the imbalance of these chemicals, stimulating and activating neural pathways of the brain that control mood so the inactive signals fire up and work again.
TMS vs. ECT
Compared to ECT, TMS can be done in an outpatient clinic and does not require anesthesia or a lengthy recovery period. ECT is conducted while the patient is under general anesthesia and uses electrical currents to induce a "therapeutic seizure" in the entire brain. It is often used for very severe cases of depression or when there is an immediate risk of suicide.
Some studies suggest the antidepressant effects of TMS are more durable than those of ECT. However, some patients, such as those with psychotic depression or severe mental health conditions, might not benefit from TMS. While patients can typically return to their activities immediately after a TMS session, patients who receive ECT might need to stay in the hospital and avoid normal activities for up to two weeks.
Who Is a Good Candidate for TMS?
The following candidates could be a good fit for TMS:
- Patients with a major depressive disorder diagnosis
- Patients who have failed two to four traditional medication trials to treat depression symptoms
- Patients who are not satisfied with the results of conventional medications
- Patients who cannot tolerate the side effects of their medications
- Patients with a diagnosis that limits their ability to take antidepressants and other medications
- Patients with depression and anxiety symptoms that interfere with daily life
Who Should Avoid TMS Treatment?
Patients who might not be a good fit for TMS include:
- Individuals with implanted metallic devices or nonremovable metallic objects in or around the head.
- Patients who have implants that are controlled by physiological signals, such as pacemakers and vagus nerve stimulators (VNS).
- Patients who are at high risk, such as those with epilepsy, a history of head injury, or other serious neurologic issues.
- Patients with acute or chronic psychotic symptoms or disorders like schizophrenia in the current depressive episode.
TMS for Specific Disorders
TMS is being studied extensively in the hopes of coming up with new treatments for psychiatry, pain management and neurological disorders. Here are both FDA-approved and potential uses for TMS.
Treatment-Resistant Depression
TMS has been FDA-approved for the treatment of medication-resistant depression since 2008. Research suggests the effectiveness of TMS in most patients with major depressive symptoms even after multiple failed courses of antidepressant medication. One study found that 63% of 38 patients responded to TMS treatment, 15% partially responded, and 42% reached remission, revealing TMS as an effective option for a major depressive disorder that does not respond to traditional treatments.
Anxiety
Researchers are currently studying the effectiveness of transcranial magnetic stimulation for anxiety disorders. Since previous studies associated generalized anxiety disorder (GAD) with excessive activity in the right dorsolateral prefrontal cortex (DLPFC), a 2022 study observed the impact of TMS on this exact brain region. The researchers found low-frequency TMS effectively improved GAD symptoms, with results sustained at one-month follow-up visits.
While further research is needed, these results show great promise in using TMS for treatment-resistant anxiety disorders.
Obsessive-Compulsive Disorder
The FDA approved transcranial magnetic stimulation for OCD in 2018. Several randomized controlled trials and real-world clinical experiences have shown TMS to be safe and effective in reducing this disorder's symptoms. In one study, over 70% of patients reached response, and over 50% achieved a sustained response after an average of 18-20 sessions.
Another study found TMS to have a moderate therapeutic effect on OCD symptom severity, with longer but fewer overall sessions predicting a more significant clinical improvement.
Post-Traumatic Stress Disorder (PTSD)
Currently, trials are looking into the effectiveness of transcranial magnetic stimulation for PTSD and complex PTSD (CPTSD). Researchers are studying its use in the areas of the brain affected by trauma, including the fear response. Some studies suggest that high-frequency TMS applied to the DLPFC might be more effective than low-frequency stimulation in improving symptoms. Other studies find that TMS might prevent the onset or worsening of PTSD symptoms for patients undergoing treatment.
Bipolar Disorder
Researchers are also looking into the use of transcranial magnetic stimulation for bipolar disorder. Since the disorder is characterized by manic and depressive episodes, early results suggest TMS may reduce the depressive symptoms of bipolar like hopelessness and lack of energy. A 2020 analysis found that 77% of people who underwent TMS for depressive symptoms of bipolar disorder met response criteria, and 41% met the criteria for remission after 25 sessions.
However, more evidence is needed to determine the best techniques for TMS, including the frequencies and exact parts of the brain to target.
Autism Spectrum Disorder (ASD)
The brains of people with autism differ from those who do not have autism, making researchers believe these areas could be a good target for TMS. More specifically, the functional connectivity between the medial prefrontal cortex and the amygdala is particularly low in patients on the autism spectrum. For this reason, researchers are exploring the use of transcranial magnetic stimulation for autism and symptoms like repetitive behaviors and social challenges.
A recent study saw improvements in social and communication skills in a TMS amygdala-targeted group compared to the DLPFC-targeted group. Still, follow-up studies are needed to understand these findings fully.
Attention-Deficit/Hyperactivity Disorder (ADHD)
Researchers are examining transcranial magnetic stimulation for ADHD as a safe, effective treatment option compared to conventional medications like psychostimulants. TMS may be able to modulate the brain circuits involved in attention, impulse control and executive functions. Studies suggest that neuroimaging and TMS can help deepen our understanding of the mechanisms that underlie attention and other brain regions involved in ADHD.
A 2023 meta-analysis reported therapeutic efficacy in TMS for improved sustained attention and processing speed. However, further research is needed to verify these findings.
What Is the Protocol for TMS Treatment?
Depending on the protocol, TMS treatment sessions can last five to 60 minutes, and patients can return to their daily activities immediately after.
The accelerated protocol is faster than standard TMS and can shorten treatment length while still being effective. For example, the McClean Hospital's accelerated TMS program involves 36 outpatient treatments condensed into five days a week. It has shown higher response rates than standard TMS, with up to 85% of people with depression responding positively. Most clinicians also consider a personalized treatment plan that addresses each patient's unique brain connectivity patterns or targets specific neural circuits related to their symptoms.
When patients arrive, they might briefly check in with the clinician before starting the stimulation process. The technician will determine the ideal electromagnetic frequency and brain regions to target by using the motor cortex as a guide. By first targeting this region, the team can determine where to place the stimulation coil and how intensely it must pulse to achieve adequate stimulation. For treatment-resistant depression, technicians can apply this data to find the dorsolateral prefrontal cortex, as it has demonstrated the greatest evidence of clinical effectiveness.
While one session might be enough to change the brain's level of excitability, most patients do not notice relief until the next few weeks of treatment.
TMS in Practice
TMS treatments are typically performed in a clinical setting, where a licensed physician maps the treatment area during the first appointment. Practitioners and clinicians must undergo theoretic and didactic competencies and learn practical skills, safety and ethics. Some clinicians must also receive a clinical degree besides an M.D., understand the device's safety protocols and participate in continuing education courses to administer TMS treatments.
All TMS technicians must complete a short course with traditional study and hands-on guidance. Applicants should have a background in healthcare, psychiatry, medicine or psychology, including an associate or bachelor's degree. They must also have experience working in a medical office or facility.
While TMS is FDA-approved to treat depression and treatment-resistant depression, OCD, migraines and smoking cessation, research is ongoing for uses like bipolar disorder, anxiety, PTSD and ADHD.
Side Effects and Considerations
Side effects of TMS are usually mild to moderate and improve shortly after a session. Common side effects include:
- Headaches.
- Scalp sensitivity.
- Scalp irritation and pain.
- Tingling, spasms or twitching of facial muscles.
- Lightheadedness.
Providers can adjust the stimulation level to reduce these symptoms or can recommend pain medications before the procedure. More serious side effects, like seizures, are extremely rare.
While the positive impacts of TMS on treatment-resistant disorders can be long-term, many patients will need to consider returning for additional treatments after a few months or years of well-being. Individuals who follow appropriate medication and lifestyle choices to maintain their improved mood may also see more prolonged therapeutic effects of TMS.
TMS Equipment and Costs
TMS machines vary widely when it comes to costs. Clinicians and practitioners can expect to pay thousands for a high-quality, well-reviewed TMS machine. You'll also want to consider the types of TMS devices and their uses:
- Repetitive TMS (rTMS): This machine uses a figure-of-8 coil to deliver a series of magnetic pulses to the brain's surface.
- Deep TMS (dTMS): This device uses a large H-coil to deliver deeper pulses into the brain. It is often used for treating OCD.
- Single-pulse TMS: The single-pulse TMS machine delivers a single magnetic pulse for diagnostic purposes.
- Theta burst stimulation (TBS): This machine uses high-frequency bursts delivered at shorter sessions than other TMS devices.
- Navigated TMS (nTMS): This machine uses imaging techniques to target specific brain areas.
Insurance Coverage
While TMS therapy may be covered by some insurance plans, like Aetna, TMS clinics and hospitals might not be as widely available as traditional treatments. Insurance might not cover treatments if the patient is at acute risk for suicide, demonstrates ongoing substance abuse, or has been diagnosed with neurological conditions like dementia, epilepsy or seizure disorders.
Future Directions of TMS Therapy
TMS therapy may venture into several directions, such as engineering new coils and technology, exploring pediatric uses and identifying functional abnormalities to treat various disorders. As we gain more knowledge of the brain's mechanisms and network interactions, researchers might also look into new stimulation targets for TMS.
Aside from bipolar disorder, PTSD, anxiety and other mental health conditions, research is delving into the uses of TMS for post-stroke brain deficits, Alzheimer's disease, schizophrenia, traumatic brain injury (TBI) and addiction.
Why Trust ICANotes for Psychiatry Software?
As a psychiatrist, you're likely always searching for the most innovative treatment options for your patients. Whether you're providing TMS therapy to your patients or another treatment approach, it's essential to maintain proper progress notes. ICANotes has the tools you need to manage the increasing complexity of healthcare documentation. Our electronic health record (EHR) was developed by clinicians with extensive behavioral health experience.
Integrating our compliant software solution allows you to streamline nonclinical tasks and meet even the most stringent standards. Practitioners can also receive unlimited mental health EHR support, as our certified experts provide training sessions to simplify psychiatric documentation and enhance patient care.
Make Documentation Easy With Our Intuitive Platform
To include TMS therapy in your practice, you need an EHR that simplifies documentation. At ICANotes, our EHR can improve compliance and reduce documentation time — freeing up time for treating patients and growing your practice. Create comprehensive progress notes, initial assessments, treatment plans and more, accelerating documentation no matter the therapy you use.
Start a free trial of ICANotes to experience our behavioral health EHR in action.
Sources:
- https://www.britannica.com/science/transcranial-magnetic-stimulation
- https://www.britannica.com/science/transcranial-magnetic-stimulation
- https://www.verywellmind.com/transcranial-magnetic-stimulations-vs-ect-380646
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10387872/
- https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.779201/full
- https://www.sciencedirect.com/science/article/pii/S0022395620310657
- https://pubmed.ncbi.nlm.nih.gov/37343662/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9193572/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10157380/
- https://onlinelibrary.wiley.com/doi/full/10.1002/brb3.1805
- https://www.thetransmitter.org/spectrum/magnetic-stimulation-for-autism-qa-with-xujun-duan/
- https://www.mdpi.com/2075-1729/14/3/329
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8195561/
- https://www.mcleanhospital.org/treatment/tms-service
- https://www.sciencedirect.com/science/article/pii/S1388245720305757
- https://iocdf.org/about-ocd/treatment/tms/
- https://ejnpn.springeropen.com/articles/10.1186/s41983-024-00825-9
- https://www.icanotes.com/free-trial/