Understanding Trauma Informed Therapy Techniques: A Guide for Clinicians
Introduction to Trauma Informed Therapy Techniques
The need for trauma informed therapy techniques stems from the reality that we all know too well - a majority of those we serve (and oftentimes many that we do not ever have a chance to serve) are navigating the impact of traumatic experiences from their past. In fact, 70% of adults in the U.S have experienced some type of traumatic event at least once in their lives. Regardless of your area of specialty, understanding and applying the principles of trauma informed care will not only enhance your practice but also allow you to incorporate these essential skills into your daily sessions, ultimately helping your clients achieve a better quality of life.
Key Takeaways
After reading this article, you should have a baseline understanding of the following trauma-informed care concepts:
- Trauma informed therapy techniques prioritize safety, trust, and empathy
- Key trauma informed care principles include safety, trustworthiness, empowerment, and cultural competence
- Understanding trauma's impact on mental health is crucial for effective treatment
- Evidence-based trauma informed approaches like EMDR, TF-CBT, and Somatic Experiencing are highly effective
- Integrating trauma informed practices involves regular training, a welcoming environment, and continuous assessment
As we navigate through the basics of trauma informed care, it is essential for clinicians to grasp the gravity of trauma work and the importance of deeply understanding these concepts prior to onboarding clients in need of trauma work.
6 Principles of Trauma Informed Care
Trauma-informed care is based on six core principles that guide and direct treatment. With these principles in mind, therapists will be able to address traumatic experiences with confidence and competency.
The 6 principles of trauma informed care are:
- Safety. Your clients have to feel safe throughout every step of this vulnerable treatment process. Not only that, but the therapist must feel the same. Dealing with trauma is an extremely intense and challenging process, so all parties must feel supported during the discomfort. Having sound supervision and institutional support is essential for this.
- Trustworthiness and Transparency. Trauma can destroy trust, for this reason, developing a trusting foundation is essential in an effective care setting. Therapists and other staff should behave in transparent and consistent ways to benefit the clients. When difficult treatment decisions are made, it should be clear why these choices are made and the expected outcomes they hope to achieve, bringing the client alongside in decision making whenever possible.
- Peer Support. Trauma symptoms should improve with good therapy, however having additional support outside of session is essential to long-term healing. Attending support groups, connecting with friends and family, and even exploring new hobbies are all part of trauma-informed care interventions.
- Collaboration. Power differences often lead to trauma and similar power differences may present in therapy. Building a model that facilitates collaboration between the client and therapist can enhance feelings of trust and the client’s perceptions about their own abilities.
- Empowerment. When a client feels a sense of control over their life, they can thrive. Increasing feelings of confidence and self-determination can increase a client’s ability to problem solve, navigate difficulties, utilize their coping skills, and become resilient.
- Humility and Responsiveness. Therapists who are practicing from a trauma-informed lens are able to determine when they are and are not the experts in a given situation. This practice of humility and awareness is essential to remaining unbiased. Within the therapy setting, a professional should constantly be working to understand their client’s experience from their perspective, remaining attuned and responsive throughout each session.

FREE Download: Trauma Informed Care Checklist
Providing care for clients with trauma histories requires empathy, skill, and thoughtful practices. Our comprehensive Checklist for Providing Trauma Informed Care is designed to guide behavioral health clinicians in creating a safe, supportive, and empowering environment for their clients.
Whether you’re already familiar with trauma-informed care or looking to deepen your knowledge, this checklist will provide the actionable steps you need to support your clients' healing journey.
Download now to ensure you’re providing the best trauma informed therapy possible and helping your clients build resilience and move toward recovery.
The Impact of Trauma on Mental Health
Trauma sources and trauma symptoms are widely diverse and will manifest differently from person to person. Some trauma may stem from a single acute source, like a car accident or an incident of physical assault, while other times trauma will develop from chronic exposure to high stress, abuse, or victimization, like military combat or abusive relationships. Some people will have just one type of trauma, while many others will have a series of varied traumatic experiences, also known as “compound trauma.”
The negative impact of trauma on a person’s physical, mental, and spiritual health is widely accepted, and whether you look at the effects from a psychological, physiological, or spiritual lens, the results are evident. It is important to remember when working with clients through a trauma lens is that both trauma experiences, as well as responses, are highly individual, requiring clinicians to view this work with nuance.
Trauma produces more than the widely expected symptoms of post-traumatic stress disorder (PTSD). It can create layers of dysfunction that shape and color the way a person interacts with the world. Some impacts of trauma include:
- Mistrust and paranoia
- High anxiety, leading to social anxiety, agoraphobia, and other phobias
- Unsuccessful, unhappy, and abusive relationships
- Educational and occupational limitations
- Mood disorders, like major depression and bipolar disorders
- Problems with income, transportation, and housing
To help better understand the complexity and individuality of these responses, we can look to experts in the field of trauma informed therapy techniques:
Two people that experienced childhood sexual abuse could present in completely different ways. One could react in an expected way by being leery of adults, appearing cold and distant to others, and struggling to enjoy relationships with anyone. The other could have what is perceived to be a counterintuitive response by becoming very sexually motivated and socially extroverted. This response can feel jarring but is actually quite common. Interestingly, this phenomenon has been widely studied. Dr. Bruce Perry noted these differences in the children he worked with in his book The Boy Who Was Raised As A Dog.
These differences could start immediately, or they could take years to fully develop and only begin to emerge when brought forth either through a developmental or situational trigger, or other major life event. Therapists working with clients can help themselves while helping their clients by being acutely aware of trauma and its impact. Without acknowledgement of the barrier, clients may quickly display a plateau in treatment without meeting their goals.
Evidence-Based Trauma Informed Therapy Techniques
When addressing trauma in therapy, it’s essential to use trauma informed therapy techniques that are not only compassionate and client-centered but also grounded in research and proven effectiveness. Trauma informed therapy encompasses a variety of evidence-based techniques that have been developed and refined to help individuals process and heal from the complex effects of trauma.
These approaches are designed to address the multifaceted nature of trauma, offering tailored strategies that can support clients in reclaiming their lives and fostering resilience.
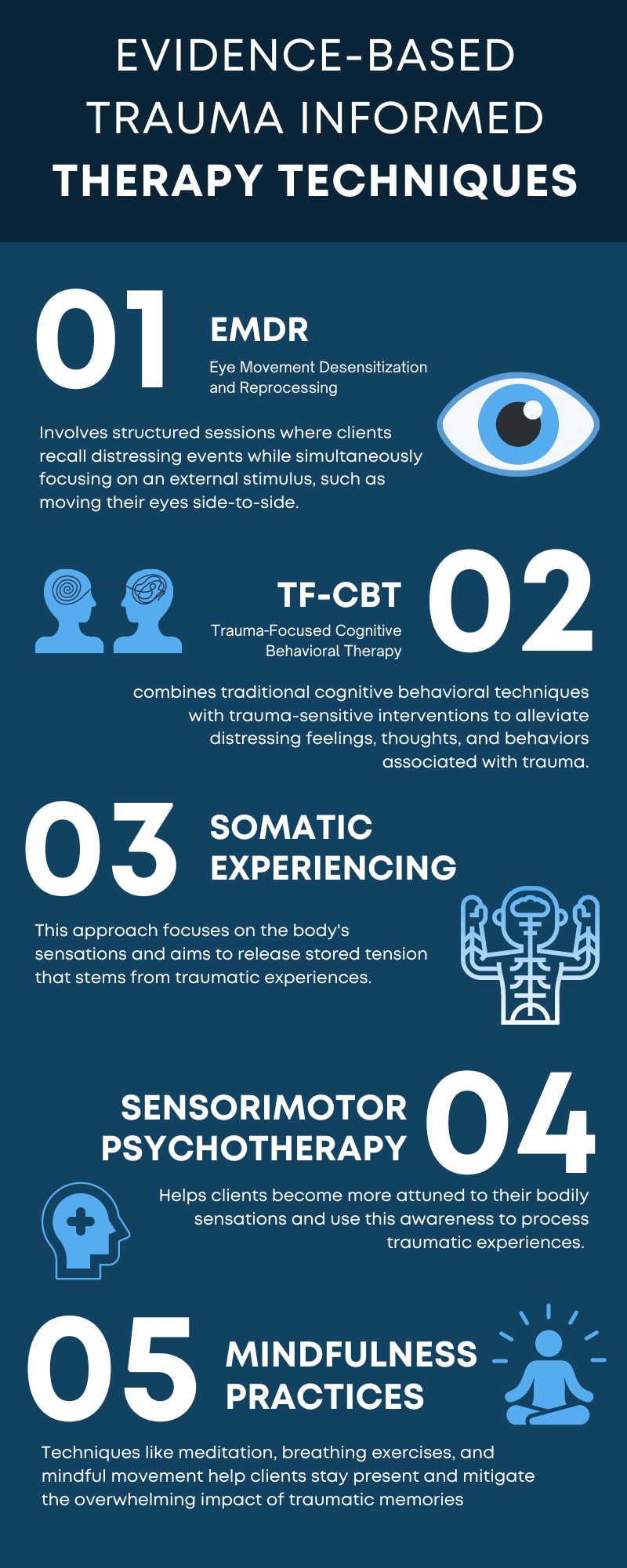
- EMDR (Eye Movement Desensitization and Reprocessing) has proven effective in reducing trauma symptoms. It involves structured sessions where clients recall distressing events while simultaneously focusing on an external stimulus, such as moving their eyes side-to-side. This process helps reprocess traumatic memories and reduce their emotional impact.
- TF-CBT (Trauma-Focused Cognitive Behavioral Therapy) offers a structured, short-term approach that is particularly beneficial for children and adolescents. It combines traditional cognitive behavioral techniques with trauma-sensitive interventions to alleviate distressing feelings, thoughts, and behaviors associated with trauma.
- Somatic Experiencing targets the physical manifestations of trauma. This approach focuses on the body's sensations and aims to release stored tension that stems from traumatic experiences. By doing so, it helps clients achieve a state of balance and improve emotional regulation.
- Sensorimotor Psychotherapy integrates somatic techniques with cognitive and emotional aspects of trauma therapy. It helps clients become more attuned to their bodily sensations and use this awareness to process traumatic experiences. This modality combines body-centric and cognitive approaches for a holistic treatment.
- Mindfulness practices are invaluable in grounding clients and reducing trauma-related stress. Techniques like meditation, breathing exercises, and mindful movement help clients stay present and mitigate the overwhelming impact of traumatic memories. Consistent practice can significantly aid in reducing anxiety and improving overall well-being.
Utilizing these evidence-based trauma informed care interventions can enhance the therapeutic relationship and support clients in their recovery journey. Each approach offers unique benefits, and often, integrating multiple methods yields the best outcomes. A trauma informed therapist may integrate multiple approaches to best meet the needs of each client, considering the specific nature and effects of their trauma.
Integrating Trauma Informed Therapy Techniques into Clinical Settings
Creating a trauma informed clinical environment involves more than just individual therapy sessions. It requires an organizational culture shift and consistent practices to support both clients and staff. Bringing trauma informed care interventions into the clinical setting can enhance your practice by creating a space that invites trust, autonomy, and transparency for every client. Though it may seem abstract at first, focusing on a few ways to represent the guidelines will get you heading in the right direction.
Some of the best ways to bring trauma informed care interventions into psychotherapy include:
- Being aware of the possibility of every client you interact with having a history of trauma, and navigating conversations and treatment modalities with that awareness.
- Providing insight to clients throughout assessment and treatment, normalizing their own personal responses to traumatic experiences.
- Being transparent about your scope of practice in trauma work. It’s crucial to communicate your level of expertise and training in trauma treatment to your client, and to recognize when certain trauma experiences or responses are beyond your capability. Referring clients to other professionals when necessary is essential to providing ethical and effective trauma care.
- Compiling and offering a list of available in-person and online trauma-focused support groups in the community to support your client in maintaining or building new peer support options.
- Encouraging the client to be engaged and involved in all decisions throughout treatment. Be sure to make recommendations and offer insights into the risks and rewards of each intervention. For example, complete direct trauma work is often distressing in the moment but incredibly beneficial in time.
- As treatment continues over time, placing more of the decision-making power on the client. This act serves to reinforce their autonomy and increases levels of trust and power.
- Reminding the client that you are there to support and provide guidance, but they are the expert on their own experience. Here, you will remain accepting of their experience and practice humility as needed.
Addressing Secondary Trauma and Burnout in Mental Health Professionals
Secondary trauma is the emotional and behavioral response to learning about or witnessing a traumatic event experienced by someone else. It can also be referred to as secondary traumatic stress, vicarious trauma, or secondary stress disorder. Secondary trauma can have negative effects on a person's life, including: job performance, professional satisfaction, intent to leave a job, relationships, and personal happiness.
Clinicians who work routinely with trauma are at risk of developing secondary, or vicarious trauma, and burnout. This is a natural result of consistent exposure to the pain and trauma that clients bring to each session, however it can and should be addressed before, during, and after the impact is felt. Addressing these issues is essential for maintaining staff well-being and effective client care.
The following measures should be put in place for all clinicians who experience exposure to traumatic stories.
- Selfcare and Boundaries: While it may feel unreasonable, it is essential for clinicians to practice selfcare both in their personal lives, as well as through setting boundaries around caseload, work hours, and client lists. As we enter this field, it can feel like we need to jump in with both feet due to the immense need we see in the communities we serve. However, striving for a balanced caseload and firm boundaries around hours can stave off secondary trauma and burnout.
- Clinical Supervision: No one is an expert in trauma informed care on day one. In fact, to be successful and ethical in trauma informed therapy, a clinician must always be learning new perspectives, approaches, studies, etc. Therapists in the trauma field need to seek out high-quality education, training opportunities, and clinical supervision to ensure they maintain high standards of care for their clients. Having weekly clinical supervisions with someone competent in trauma informed therapy and frequent check-ins with co-workers or colleagues can drastically improve your skills and is essential to ensuring checks and balances in the therapeutic process.
- Continuous Clinical Training: Continuing to improve your clinical knowledge of trauma work can mitigate the risk of burnout and secondary trauma by routinely building clinical capacity and skills. There are countless training opportunities for people interested in growing their trauma informed care knowledge. Eye-movement desensitization and reprocessing (EMDR), trauma-focused cognitive behavioral therapy (TF-CBT), and other specific treatment interventions can add to your repertoire of available therapy tools.
Ethical Considerations in Trauma Informed Therapy
Ethical issues play a significant role in trauma therapy. Upholding confidentiality, ensuring informed consent, and maintaining professional boundaries are vital for ethical conduct.
Confidentiality is crucial in trauma-informed practices. Clients need to trust that their sensitive information will be kept private. Any breaches of confidentiality can significantly damage the therapeutic relationship and exacerbate trauma symptoms.
Informed consent must be comprehensive. Clients should have clear explanations of the trauma-informed care interventions, potential risks, benefits, and alternatives. This transparency fosters trust and empowers clients to make informed decisions about their treatment.
Maintaining professional boundaries ensures ethical conduct in trauma therapy. Boundaries help create a safe and predictable environment, which is essential for trauma survivors who often experience boundary violations. Clear professional lines prevent the risk of re-traumatization and maintain the integrity of the therapeutic relationship.
Cultural sensitivity and humility are also crucial. Trauma affects individuals differently, shaped by cultural, social, and personal contexts. Therapists must approach each client with an open mind, respect diverse backgrounds, and acknowledge their own potential biases.
Finally, ethical decision-making processes need to prioritize client safety and autonomy. When faced with ethical dilemmas, the well-being and rights of the client should be at the forefront of any decision-making. This involves continuous ethical education and reflective practice to navigate the complexities of trauma therapy responsibly.
Addressing these ethical considerations ensures that trauma informed therapy upholds the highest standards of care, protecting and empowering clients throughout their healing journey.
Trauma therapy is not an add-on service clinicians can learn through trial and error. It is a specialty field that needs to be studied and well understood before taking on a single client for trauma work. Even after this understanding has been established, it is essential for therapists to never attempt to work with trauma clients in a vacuum. Supervision and continuing education will ensure you know what you don’t know, alleviating ethical violations and irreparable damage to individuals seeking your care.
By understanding the 6 principles of trauma informed care -- safety, trust, support, collaboration, empowerment, and humility -- therapists can improve their skills, and support clients in improving their symptoms.
Documenting Trauma Informed Care Interventions
ICANotes software can help with documenting the complexities of working with trauma. As a clinician, you know that it's essential to maintain accurate documentation that is tailored to each client. With the right documentation tools from ICANotes, you can create unique progress notes quickly and effectively after every session – ensuring you’re prepared, organized and ready to best help your client at their next session.
Outside of helping you create progress notes, ICANotes behavioral health software makes it easy to improve compliance and bill more effectively, ensuring you get to spend focused, ample, and productive time with your patients. Schedule a demo today or start your free trial to see how ICANotes can support you in providing the most effective, high quality care possible.
About the Author

Kaylee, a certified grief counselor and social worker, has dedicated the past decade to reshaping our understanding and support of grief. With experience at a nonprofit hospice, she's empowered individuals to navigate their grief journeys, recognizing that loss extends beyond death. As an author, speaker, and event organizer, Kaylee fosters spaces for acknowledging and embracing life's most challenging moments. Her work has been featured across various media, amplifying voices and broadening awareness of the diverse sources of grief in our lives.
Recent Posts
Sources
- Trauma-Informed Care Implementation Resource Center. (2024). What is Trauma-Informed Care?
- University at Buffalo. (2024). What is Trauma-Informed Care?