Navigating the Challenges of Treating Co-Occurring Disorders
An individual who has both a mental health condition and a substance use disorder (SUD) is said to have a co-occurring disorder. This occurrence affects more than 21 million adults in the United States. However, these conditions can be challenging to treat because symptoms often overlap. If a co-occurring disorder is not properly diagnosed, it creates an additional barrier to treatment for patients who may already find it difficult to seek help.
As a therapist or behavioral health clinician, it's important to understand the impact that mental health co-occurring conditions can have on treatment and recovery. With the right tools and a multidisciplinary team approach, you can create effective treatment plans. This guide will help you understand how to deliver the best possible care for patients with co-occurring disorders, from comprehensive assessments and accurate documentation to effective collaboration.
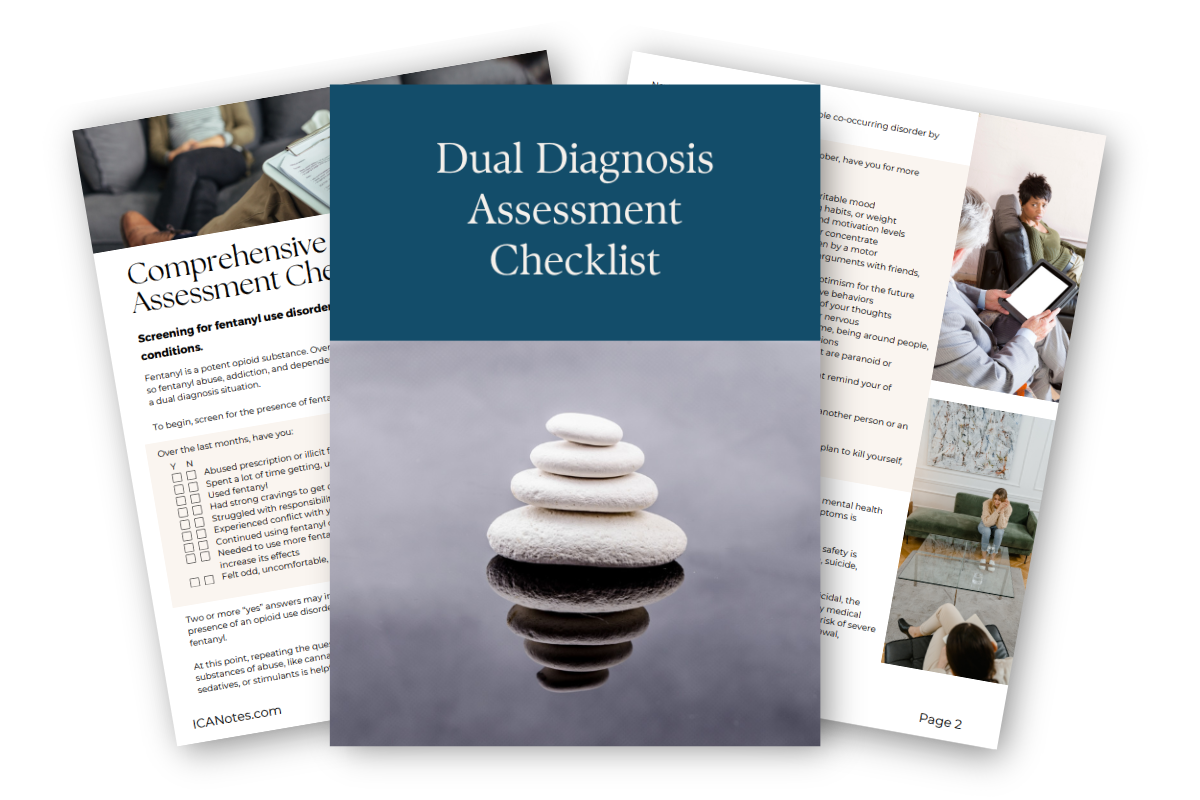
Instant Download: Comprehensive Dual Diagnosis Assessment Checklist
Download this screening for opioid use disorder and co-occurring mental health conditions.
Understanding Co-Occurring Disorders
Co-occurring disorders, also known as concurrent or comorbidity disorders, affect individuals with SUDs and psychiatric conditions. According to the Substance Abuse and Mental Health Services Administration, individuals with a mental health condition are more likely to experience substance use disorder than those without. This is because some individuals may misuse substances like drugs or alcohol as a way to self-medicate to relieve or reduce their symptoms.
Likewise, those with a substance use disorder are at a higher risk for developing a mental health condition. Because substance abuse and mental health conditions can have many underlying causes, however, it can be difficult to identify the root cause of these coexisting conditions.
For example, exposure to stress and trauma and genetic predispositions can contribute to serious mental health conditions and substance abuse issues. Other potential causes of co-occurring disorders include peer influences, lack of social support, adverse childhood experiences and environmental stressors.
The most common mental health conditions associated with SUD include:
- Anxiety and mood disorders.
- Attention deficit hyperactivity disorder (ADHD).
- Bipolar disorder.
- Conduct disorders.
- Major depressive disorder (MDD).
- Post-traumatic stress disorder (PTSD).
- Schizophrenia.
It's estimated that more than one in four adults who live with serious mental health conditions also has a substance abuse problem.
Dual Diagnosis vs. Co-Occurring Disorders
Co-occurring disorders are not necessarily the same thing as a dual diagnosis. Co-occurring disorders specifically refer to at least two or more mental health conditions that exist at the same time, typically accompanying or as a result of substance abuse. A dual diagnosis refers to two diagnoses that are completely separate.
For instance, having diabetes and high blood pressure could be considered a dual diagnosis. However, an individual who misuses substances to self-medicate and develops a mental health disorder would have co-occurring disorders because the two conditions are very closely linked and would need to be treated together. This distinction is vital to understand and can make all the difference during treatment and recovery for your patients.
Challenges of Treating Co-Occurring Disorders
Every individual has unique experiences and symptoms, including those with co-occurring disorders. However, certain barriers can make it challenging for patients to seek help and receive effective treatment. Here are some factors to keep in mind when caring for a patient with a combination of conditions or symptoms.
1. Diagnostic Challenges
Co-occurring disorders are known for being difficult to diagnose. Many symptoms and behaviors of substance abuse and mental health conditions overlap, which makes proper identification a challenge. As with symptoms, the root causes of each condition can also be intertwined. Additionally, mental health symptoms can sometimes be masked by substance abuse.
A comprehensive assessment for both mental health conditions and SUDs is required for accurate diagnosis and treatment planning. Another consideration for accurate diagnosis is how differently co-occurring disorders can look in patients. For example, an individual with SUD and generalized anxiety will have different symptoms than someone with SUD and schizophrenia.
With that in mind, some common symptoms of co-occurring disorders can include:
- Lack of motivation.
- Sudden mood swings.
- Changes in sleep or appetite.
- Increased risk-taking or secretive behavior.
- Significant changes in personality or behavior.
- Neglecting professional or personal responsibilities.
- Social withdrawal.
- Financial or legal problems.
- Worsening mental health due to ongoing substance abuse.
- Worsening substance abuse issues to manage a mental health condition.
If your patient struggles with misusing substances or has been diagnosed with a SUD, it may be worth considering whether their symptoms reflect that of a co-occurring disorder.
2. Mental Health Stigma
The stigma associated with mental health and addiction is a significant barrier to receiving care. Individuals who may be aware they are struggling may isolate themselves due to shame rather than seek help. Although addiction has been classified as a disease, it is often treated otherwise in social scenarios.
Some individuals may blame themselves for their lack of willpower in overcoming substance abuse. The effects of stigma can result in a diminished quality of life, delayed diagnosis and treatment, and increased morbidity.
3. Treatment Resistance
Patients with SUD commonly exhibit resistance, denial and low motivation. Having co-occurring disorders can contribute to a patient's treatment resistance, especially when it comes to their motivation to engage in or adhere to therapy interventions. The presence of a mental health disorder combined with substance abuse can complicate the recovery process.
4. Financial and Systemic Barriers
Patients who do seek treatment also have to deal with the financial toll of receiving services, particularly if they do not have insurance. The financial barrier can be difficult to overcome, and long-term treatment may not be a sustainable option. As a clinician, you may also experience billing issues if your patient has not been correctly diagnosed for their co-occurring disorder.
Alternatively, some behavioral health facilities may only treat mental health conditions, not substance abuse, which can create more complications. In many places, addiction and mental health services are considered separate, which adds to the challenge for patients seeking help.
A comprehensive assessment is necessary to coordinate care and refer patients to the services they need and can afford.
5. Potential for Exacerbation
When treating a patient who has two or more mental health conditions, it's important to look for signs of exacerbation. Clinicians must recognize these conditions have a reciprocal relationship. For example, treating the root cause of substance abuse in a patient without considering its interconnectedness with their depression may increase their risk of relapse. In fact, individuals with mental health conditions have a higher risk of adverse outcomes like overdosing.
Alternatively, treating someone for depression when they also engage in substance abuse may cause a setback in their mental health. Mental health disorders and substance abuse function in a vicious cycle and can reinforce each other. They should be treated concurrently with a comprehensive treatment plan.

Strategies to Overcome Treatment Barriers
Your role as a dedicated behavioral health professional is vital. Here's what you can do to help patients seek and adhere to treatment:
- Build supportive networks: Access to care remains a significant barrier for many. You can help by providing community resources to your patients or connecting them with social supports, such as group therapy for those also in recovery. Simply helping them celebrate their achievements can help them stay motivated during treatment.
- Reduce the stigma: Whether you're a psychologist, substance abuse counselor or therapist, it's imperative to create a safe, nonjudgmental environment for all patients. Those who struggle with addiction may not want to disclose their experiences if they do decide to seek support. Be patient and give your clients time to open up.
- Integrated care: Integrated treatment models can better address co-occurring disorders than treating mental health and substance abuse separately. While each condition has its own set of symptoms and needs, the nature of a co-occurring disorder is that both conditions are inextricably linked. Seamlessly combining mental health services with substance abuse treatment can result in more favorable outcomes.
- Interdisciplinary collaboration: Collaboration in multidisciplinary treatment teams ensures that patient's needs are being met. Those living with co-occurring disorders will benefit from a collaborative team of case managers, therapists, psychiatrists, nurses and rehabilitation specialists who cross-train each other on a patient's progress for a continuum of care.
- Dual-focused interventions: Therapeutic interventions for co-occurring disorders are most effective when they involve a combination of treatment modalities, including medication, lifestyle modifications, psychotherapy and support groups. It's necessary to tailor treatment plans to address both the substance abuse and mental health conditions of the individual.
How to Build Effective Treatment Plans for Co-Occurring Disorders
Though there are several barriers and challenges when it comes to treating patients with co-occurring disorders, there are plenty of steps you can take as a behavioral health clinician to make ongoing treatment modalities more effective.
1. Use an Integrated Treatment Approach
Keep in mind that if an individual has more than one mental health condition, it will likely take more than one typical treatment method for them to see progress. Due to the nature of co-occurring disorders, an integrated approach can help you address both conditions in your patients and lead to improved patient outcomes.
An integrated treatment plan often includes a combination of treatments, such as medication and psychotherapy, and provides one consistent message throughout the recovery process. Consider an integrated treatment plan as a holistic approach, where you and other providers will consider many different factors that may affect a patient's needs.
Components of effective integrated treatment for co-occurring disorders include:
- A multidisciplinary team.
- Integrated treatment specialists.
- Motivational interventions.
- Substance abuse counseling.
- Group treatment for co-occurring disorders.
- Family interventions.
- Connection to resources for safe housing, proper diet and exercise.
- Interventions to avoid high-risk behaviors.
- Evaluation and referral to secondary interventions, if needed.

2. Develop Personalized Treatment Plans
Though all patients deserve a personalized treatment plan, those with co-occurring disorders can especially benefit from tailored plans that fit their needs and improve their quality of life. A personalized treatment plan considers the patient's physical health, family history, personal goals and symptoms. Personalized treatment plans take a comprehensive approach by treating the whole person, including their physical, mental and emotional health. This approach can help motivate individuals who may resist engaging in treatment because they feel ashamed of their struggles or diagnoses.
By identifying reasonable recovery goals and life changes, your patients may feel more empowered. Additionally, a tailored treatment plan considers their unique lifestyle and needs and allows for their voice to be heard. Instead of isolating their disorders or symptoms, a personalized treatment plan can continually assess and adapt their treatment based on their progress.
3. Implement Collaborative Care Strategies
Interdisciplinary collaboration is key for any effective treatment plan. By implementing a collaborative care model at your practice, you and other providers can proactively address your patient's needs. The collaborative care model consists of five core components:
- Patient-centered care
- Population-based care
- Measurement-based treatment
- Evidence-based care
- Accountable care
Coordinating care across disciplines can help your team communicate effectively to treat your patient physically, emotionally and mentally. A vital aspect of collaborative care strategies and adapting interventions is maintaining accurate documentation to understand why treatment has been adjusted.
4. Administer Evidence-Based Therapies
As previously noted, mental health and addiction treatment are often considered separate services. However, those with co-occurring disorders require a combination of these services to effectively treat their underlying causes and improve their chances of recovery. Here are some of the evidence-based treatment options for co-occurring disorders.
- Detox from drugs or alcohol
- Contingency management
- Cognitive behavioral therapy (CBT)
- Dialectical behavioral therapy (DBT)
- Motivational interviewing (MI)
- Eye movement desensitization and reprocessing (EMDR)
- Peer support or group therapy
- 12-step programs
- Relapse prevention
- Partial hospitalization programs (PHPs)
- Intensive outpatient programs (IOPs)
- Medication management
Remember, the precise treatment modality will depend on the severity of your patient's condition. Treating co-occurring disorders is a highly individualized and complex process that often involves a unique combination of therapy, medication and support groups. As a clinician, your most important job is to make your patient feel safe and welcome in your practice. Maintaining accurate, clear documentation can also make treatment more efficient when working within a multidisciplinary team.
Why Trust Us?
Providing quality care to your patients is your top priority. If you're spending too much time at your desk writing notes by hand or feel that your documentation results in too many bottlenecks, it's time to switch to a clinically robust charting solution.
At ICANotes, we strive to make behavioral health documentation comprehensive, sophisticated and fast so that you can focus on providing holistic care to your patients. ICANotes was founded in 1999 to provide support to behavioral health clinicians and organizations as they navigate obstacles within the industry.
Our electronic health record (EHR) was built by clinicians for clinicians. Designed by those who understand the challenges you face, ICANotes is your ultimate resource for charting, billing and collaborating with your patient's care team.
Improve Treatment Efforts for Co-Occurring Disorders With ICANotes
Patients with co-occurring disorders face many challenges when it comes to accessing affordable treatment and community resources. As a behavioral health clinician, you can help your clients on their mental health journeys by implementing integrated and collaborative treatment strategies. As the behavioral healthcare environment becomes more and more complex, it's essential to have a resource that can help you improve clinical documentation legibility and pass regulatory scrutiny.
With our EHR, you can quickly create accurate documentation for all types of therapy sessions. Whether you're doing an initial intake, creating a treatment plan or sharing notes with other authorized providers, ICANotes makes it easy to complete your notes and improve patient outcomes. Start your free trial today, or request a live demo to see why so many clinicians trust our software!
Register for a free 30-day trial now -- no credit card required!
Linked Sources:
-
- https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/co-occurring-disorders
- https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/co-occurring-disorders
- https://nida.nih.gov/research-topics/co-occurring-disorders-health-conditions
- https://www.samhsa.gov/mental-health/mental-health-substance-use-co-occurring-disorders
- https://www.samhsa.gov/mental-health/mental-health-substance-use-co-occurring-disorders
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10220277/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9434658/
- https://www.icanotes.com/2024/06/01/increase-participation-in-group-therapy/
- https://www.cdc.gov/mmwr/volumes/73/wr/mm7334a3.htm
- https://www.icanotes.com/2022/06/03/life-skills-activities-for-group-therapy/
- https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-022-00302-9
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10889170/