Understanding and Addressing Depression in the Elderly
For clinicians working with the elderly population, special attention should be paid to the unique factors experienced at this particular stage of life that increase an individual’s risk of depression. While generalized depression in the elderly can occur, this blog will explore the unique complexities that older adults navigate in later life that pose a heightened risk for depression including declining health, loneliness, and grief.
According to the World Health Organization (WHO), global rates of depression among older adults ranges between 10-20% [1]. However, due to the complexities that older adults often face, including co-occurring physical and mental health conditions and potential memory issues, among other things, it is estimated that 50% of elderly individuals living with depression remain undiagnosed.
Recognizing Depression in the Elderly
Geriatric mental health is deeply important for improving quality of life for clients over the age of 60. Depression is the most commonly observed and diagnosed mental health disorder among older adults, creating additional need for support and intervention as individuals navigate later life [1]. In addition to the general challenges associated with aging, i.e. changes to health and stamina, loss of friends and family, and independence, many elderly individuals also struggle with major life changes which can increase their risk for depression. These life changes may include but are not limited to chronic pain or terminal illness diagnoses, loss of a spouse or partner, financial instability, and elder abuse [2].
Factors Contributing to Geriatric Depression
As previously mentioned, the elderly are at a high risk of depression due to a myriad of factors present as a result of their advanced age including grief and loss, loneliness and isolation, and biological and environmental factors. While each of these factors may be present across the lifespan, the elderly experience these issues at higher rates.
Grief and Loss
When considering grief and mourning, it is important to note that the period of mourning is an incredibly impactful and exhausting experience. For the elderly who may be experiencing loss at a higher rate (i.e. friends, family, spouse), repeated loss poses a higher impact, potentially resulting in prolonged or complicated grief [3]. Complicated grief, unlike typical grief, is associated with longer periods of mourning as well as a deeper and more prolonged sense of hopelessness. Rates of complicated grief within the general population is around 4.8%, rates for those aged 75-85 are at a higher risk, and are more severe when co-occurring alongside anxiety (17.2%) or depression (9.7%) [3].
Loneliness and Isolation
Across the lifespan, social connectedness is a highly influential factor in relation to life satisfaction. Social connectedness is correlated with lower risk of health issues, suicidality and early death [4]. Older adults are at an increased risk of loneliness and isolation as a result of life circumstances, loss history, and poor health. Transversely, individuals who are socially isolated are also at a higher risk for longer hospital stays, higher rates of re-admittance to the hospital, and early death.
Health conditions are also linked to social isolation which can further exacerbate depressive symptoms including:
- Alzheimer’s Disease or Dementia
- High Blood Pressure
- Heart Disease
- Weakened Immune Function
- Cognitive Decline
Biological and Environmental Factors
While each of the previous factors listed create a high risk of depression in the elderly, there are also biological and environmental factors that contribute to this risk. It is important to note that while each of these factors alone may contribute to the development of depression, the elderly experience compounding risk factors that by virtue increase their overall risk for developing depression.
Biological Risk Factors [1]
- Family history of depression
- Health conditions that may lead to depression
- Hormonal changes
- Brain chemistry
- Medications
Environmental Risk Factors [1]
- Air or noise pollution
- Poor housing quality
- Neighborhood environment
- Social isolation
- Major life transitions (loss of a spouse, relocation, financial changes)
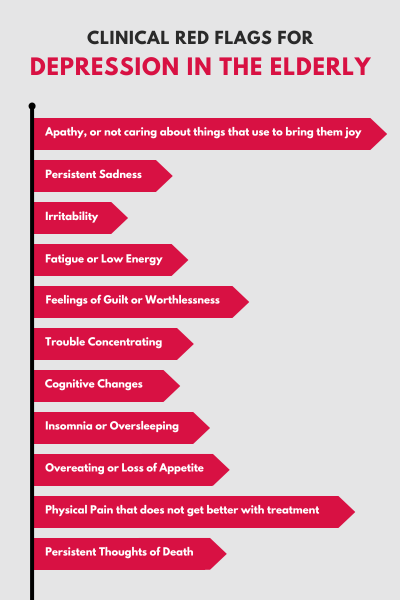
Clinical Red Flags for Depression in the Elderly
As a clinician working with this special population, it is important to maintain awareness of the high risk of depression in conjunction with major life changes. Signs of depression in the elderly include:
- Apathy, or not caring about things that use to bring them joy
- Persistent Sadness
- Irritability
- Fatigue or Low Energy
- Feelings of Guilt or Worthlessness
- Trouble Concentrating
- Cognitive Changes
- Insomnia or Oversleeping
- Overeating or Loss of Appetite
- Physical Pain that Does Not Get Better with Treatment
- Persistent Thoughts of Death
Treatment Options for Depression in the Elderly
Clinicians working with the elderly may feel the weight of a depressive diagnosis, given the internal and external factors at play, there is always hope for improving an individual’s quality of life through targeted interventions that work to mitigate the risk factors and provide a sense of hope.
Psychotherapy
Formal mental health support is warranted when depressive symptoms are showing a marked impact on the individual’s daily life and investment in future planning. Clinicians can employ a variety of interventions based on the individual in the room with them. These interventions can include Cognitive Behavioral Therapy, Narrative Therapy, Acceptance and Commitment Therapy, and Grief Counseling. These interventions should be reflective of the needs of the client.
Antidepressants for Elderly Clients
Medications may be warranted in conjunction with formal therapy [5]. Psychopharmacology, specifically the use of SSRIs, has been proven to be an effective treatment for major depression in the elderly population. Should you choose to support your client in exploring these options, it is important to consult a prescribing physician to assess, prescribe, and monitor the use of these methods to ensure it remains a safe and effective option.
Lifestyle Interventions
Combating the risk factors for older adult depression should include support around lifestyle changes that can mitigate the factors that often contribute to depression. This may include personal changes to their diet, physical activity, and hygiene practices. Additionally, it is important to encourage increased social engagement to reduce social isolation and loneliness, including social engagement programs, reaching out to family and friends, attending church services, etc.
The elderly community is a vital and vibrant population that deserve attention and support to ensure their final years provide quality and enjoyment. While this special population tends to be left behind, clinicians with a specific focus on the geriatric community have an incredible opportunity to create real, needed change to an individual's life satisfaction.
The ICANotes Behavioral Health EHR can be a game-changer for clinicians working with the elderly population. Its intuitive clinical content templates and button-driven navigation enable the creation of comprehensive, personalized notes in just minutes, ensuring thorough documentation that meets the highest standards. These templates guide clinicians through the complexities of geriatric care, such as assessing depression and tracking co-occurring conditions, while automatically suggesting the highest reimbursable codes to maximize revenue. With built-in tools for compliance and patient care, ICANotes reduces the time spent on administrative tasks, giving clinicians more opportunities to focus on their patients. Clinicians interested in experiencing these benefits can try ICANotes free for 30 days to see how it can improve efficiency and quality of care.
Sign up for a free trial (no credit card required) or schedule a demo to explore how ICANotes can support your work with clients.
About the Author

Kaylee, a certified grief counselor and social worker, has dedicated the past decade to reshaping our understanding and support of grief. With experience at a nonprofit hospice, she's empowered individuals to navigate their grief journeys, recognizing that loss extends beyond death. As an author, speaker, and event organizer, Kaylee fosters spaces for acknowledging and embracing life's most challenging moments. Her work has been featured across various media, amplifying voices and broadening awareness of the diverse sources of grief in our lives.
Recent Posts
Sources
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8684627/
- https://www.ncoa.org/article/how-common-is-depression-in-older-adults/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3822663/
- https://www.nia.nih.gov/health/loneliness-and-social-isolation/loneliness-and-social-isolation-tips-staying-connected
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3314291/

