Blog > Practice Management > Utilizing Practice Management Tools to Streamline Your Mental Health Documentation Workflow
Utilizing Practice Management Tools to Streamline Your Mental Health Documentation Workflow
Paper-based documentation can slow down your mental health practice and increase the risk of costly errors. This blog explores how practice management tools like EHR systems can streamline everything from intake forms and note templates to billing and secure data storage. Learn how to simplify your workflows, improve patient care, and boost your practice’s efficiency.

Last Updated: April 23, 2025


What You'll Learn
- How practice management tools like EHRs can streamline documentation, reduce errors, and save time.
- Ways to digitize intake forms and automate note-writing using customizable templates.
- How integrated billing features can improve claim accuracy and speed up reimbursement.
- Best practices for securely storing client data and maintaining HIPAA compliance.
As a therapist, psychologist, counselor, psychiatrist or practice administrator, you deal with a lot of paperwork. From writing notes after each session and creating treatment plans to handling billing, you collect, organize and store crucial information about your clients daily.
Just over 30% of mental health practices still use manual methods for these tasks. Beyond being an administrative burden, paper-based processes typically lead to inefficiencies, inaccuracies and errors that can impact the care delivered. Fortunately, practice management tools can help streamline various administrative duties. Learn how you can use these platforms to simplify and improve your documentation workflows.
What Are Behavioral Health Practice Management Tools?
Practice management tools are software solutions that optimize, automate and centralize key mental health practice processes. These solutions boost operational efficiency, reduce administrative workloads and improve the quality of patient care.
An advanced electronic health record (EHR) system, like ICANotes, offers features that support complete, accurate, organized, legible and compliant documentation. With EHR software, you can effortlessly create and securely store clinical notes, treatment plans and other vital documents. Some platforms include additional functionality, like billing, payments, telehealth, scheduling and calendar management, creating one centralized hub for critical tasks.
How to Streamline Mental Health Documentation With Practice Management Tools
Take a look at four core features of EHR systems and how you can use mental health software to digitize and optimize your workflows.
1. Digital Intake Forms
Intake forms are foundational documents used to collect personal, medical and psychological information from new patients to inform assessment sessions. While patients have traditionally filled out these forms by hand, paper-based methods are time-consuming and have a high potential for errors due to issues like illegible handwriting. Practice management systems like EHR software allow you to digitize your practice's intake processes with electronic forms, helping you overcome these challenges.
You can create customized digital intake forms tailored to your practice's specific needs and specialization. You can also convert any existing forms into electronic versions, making updates as necessary. Simply share these forms with new clients before their appointments, either through your patient portal, via an email link or by embedding intake forms on your practice's website. Patients can complete these forms from the comfort of their own homes on any device and spend less time in waiting rooms.
Digital intake forms also speed up administrative processes by prepopulating data directly into your EHR, eliminating the need for manual data entry tasks, inefficient paper-based storage systems and manual file retrieval. As a result, front desk staff will have more capacity to focus on providing attentive patient care and creating a supportive environment.
2. Preconfigured Note Templates
Accurate and comprehensive note-writing is essential for mental health professionals. Your clinical notes provide a crucial record of each patient's journey, documenting progress from their first appointment to the moment they achieve their therapeutic goals and informing ongoing treatment plans. However, manual note-writing is time-consuming and can lead to inconsistencies.
With EHR software, preconfigured templates for various types of therapy notes help you save time and ensure consistency by offering a structured format. Unorganized clinical notes containing irrelevant details can be tough to comprehend. Preconfigured formats like Subjective, Objective, Assessment and Plan (SOAP) or Behavior, Intervention, Response and Plan (BIRP) provide a standardized approach to writing progress notes, making it much easier to include all the necessary information.
The ability to customize data entry fields and update categorizations allows you to tailor templates to suit your practice's focus area. Whether you specialize in psychiatric and substance abuse counseling or group and family therapy, templates can help you create detailed and compliant notes more efficiently. Such tools enable you to focus on providing quality patient care without worrying about omissions or errors.
3. Automated Billing
Proper documentation is vital for private practice billing, as your patients' medical records determine the billable services. These records provide the required support for the diagnoses and procedure codes submitted to insurance. However, mental health billing can be complex.
Many private mental health practices operate with limited administrative resources, which can result in unintentional mistakes. These errors typically lead to claim denials and delayed payments, compromising your practice's financial stability. Intricate and repetitive billing processes can reduce the time and energy available to focus on patient care and make you feel overworked.
The mental health billing features of EHR software offer a solution. Such platforms can simplify your processes and improve the accuracy of your documentation, minimizing the time spent resolving rejected claims. Through the automation capabilities of these platforms, you can maximize revenue by rapidly processing claims, all while reducing your practice's administrative workload.
The following documentation tasks can all be streamlined through an EHR with an integrated billing platform:
- Generating CMS forms, patient statements, and superbills
- Submitting claims electronically
- Keeping track of authorizations
- Automating remittance posting
- Creating reports
- Customizing patient statements
- Facilitating secondary claim submissions for clients with additional insurance plans
4. Secure and Compliant Data Storage
Your mental health practice handles sensitive data daily, from patients' health histories to treatment plans. Paper-based records are vulnerable to loss or damage — losing a patient's chart can make it challenging to continue treatment. Additionally, paper records are not secure, and it is much easier for people to gain unauthorized access.
Mental health practices have both an ethical and legal obligation to ensure data security. Converting existing documents to digital formats, adopting electronic processes, and storing and organizing information with EHR software can make it much easier to uphold this duty. The following tools ensure secure storage:
Audit trails: Keep track of every user who logs into the system.
Access controls: Allow specific privileges to certain users based on their roles.
Encryption: Protect sensitive information by converting it into an unreadable format.
User authentication: Verify users' identities with usernames and password protection.
This way, you can keep your patients' information safe while complying with privacy laws. Comprehensive data security can help prevent breaches, protecting patients' privacy and your practice’s reputation. With EHRs, only authorized staff can easily access the relevant digital records.
What Are the Benefits of Streamlined Mental Health Documentation?
Streamlining mental health documentation with EHR software offers several significant benefits for your practice:
Improved efficiency: Some practitioners spend twice as much time on documentation as they do with patients. Streamlining these workflows alleviates the administrative burden by reducing the time you or your team spend on tasks like data entry or paperwork, giving you more time to focus on patients. It also helps you complete notes and reports more quickly.
Enhanced accuracy and consistency: Digital and automated processes lower the risk of mistakes with paper-based systems and manual data entry, such as misreading illegible handwriting or inaccurately entering information. Standardized billing practices, intake forms and note-writing procedures also ensure consistency.
Better patient care and decision-making: Beyond having more time for patients, streamlined workflows can help you provide them with a higher quality of care. Spending less time on documentation means you can be more attentive and save your energy for mission-critical work. Plus, having quick access to the information you need when you're in session or creating treatment plans will help you make well-informed decisions more quickly.
Improved revenue cycle management: Complete and accurate documentation can minimize the risk of denied claims and delayed payments, improving your cash flow. Faster and more reliable billing processes through automated billing also mean you get paid more quickly. Streamlined documentation workflows can also boost revenue by maximizing reimbursement while cutting administrative expenses.
Why Trust ICANotes for Mental Health Practice Management Tools?
ICANotes offers the most clinically robust EHR platform, specifically designed to meet the needs of behavioral and mental health professionals in both outpatient and inpatient settings. We developed this solution with a wide range of features to help you streamline documentation workflows, improve your practice's regulatory compliance and enhance the quality of patient care.
From mental health note templates to billing software, you can trust ICANotes for easy-to-use yet comprehensive practice management tools. Our solutions are ready to use out-of-the-box, providing instant access to a quick, sophisticated documentation system that meets the most demanding standards. We also offer training sessions and classes to help you accelerate your use of our software tools.
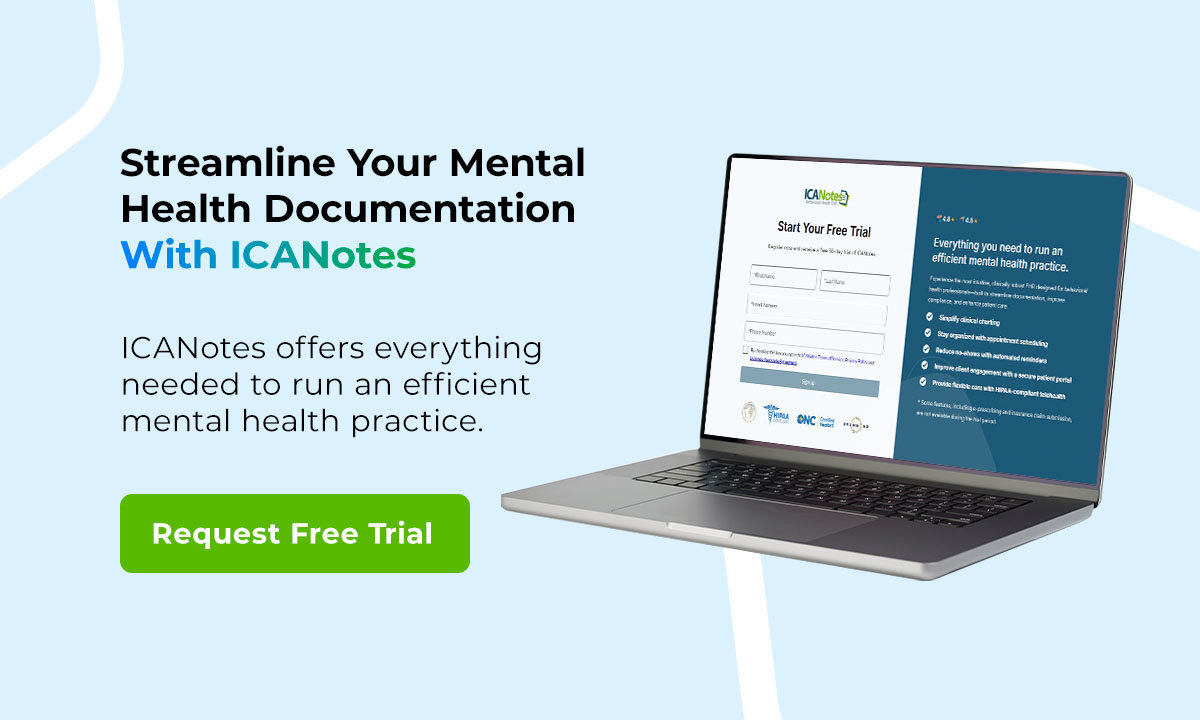
Streamline Your Mental Health Documentation With ICANotes
Designed by a clinical psychiatrist for clinicians like you, ICANotes offers everything needed to run an efficient mental health practice. Learn more about how we can streamline your documentation and practice management workflows by experiencing our software's capabilities. Schedule a live demo or request a free trial today.
Get Your Free 30-Day Trial (no credit card required!)
Related Posts
Lindsay Rutter, MA, NCC, LPC, is a Licensed Professional Counselor with a Master’s Degree in Clinical Counseling. She has nearly 15 years of clinical and supervisory experience with extensive knowledge of mental health diagnoses, their etiology and evidence-based treatments. Lindsay is the Clinical Director of a nonprofit community mental health center and the owner of a private practice in Chester County, PA.






