PIRP vs GIRP vs BIRP Notes - What's the Difference?
As a behavioral health clinician, you're always writing notes during and following sessions. Whether a patient is dealing with depression, anxiety, a substance use disorder or is undiagnosed, accurate and detailed notes are necessary for their treatment. Progress notes facilitate the treatment process and allow for effective communication. Notes propel a patient's trajectory through treatment and help to ensure the best outcomes.
Though they serve this common purpose, progress notes can take on many different forms. A mental health professional might aim to identify and solve a specific problem, work toward achieving a specific goal or characterize a patient's attitude and behavior. The approach to note writing has a significant effect on the treatment process. Understanding different progress note formats is vital for anyone in a clinical setting.
The Role of Progress Notes
Progress notes are medical records regarding a patient's status or achievements throughout their treatment. Such notes are vital for behavioral health purposes and addiction treatment. They are the record of events, serving as the history of a patient's condition and progress.
Note-writing is an integral part of mental health services. It facilitates a treatment plan, allows clinicians to remember key information and ensures the best continued care. It also strengthens communication between the various healthcare professionals who may be involved with one patient's care. Progress notes keep a patient's care on the right path. Different types of clinical notes serve varied purposes. Most progress notes take on one of three forms, which are:
- PIRP: PIRP stands for problem, intervention, response, plan.
- GIRP: GIRP stands for goal, intervention, response, plan.
- BIRP: BIRP stands for behavior, intervention, response, plan.
To be effective, progress notes need to be easy to interpret, complete and concise. In some cases, abbreviations, errors or misspellings can hinder notes' effectiveness. The PIRP, GIRP and BIRP formats can help healthcare professionals improve their note writing. Each focuses on a different aspect of care — problem-solving, goal achievement or behavioral observation, respectively.
Download our Free Guide to Writing Better Notes
This resource is essential for any clinician looking to save time while maintaining high standards in documentation. This guide covers streamlined note-writing techniques, and best practices for organizing progress notes and treatment plans.
Why Do Note Formats Matter?
The main difference between PIRP versus BIRP notes and BIRP versus GIRP notes is the overarching point of emphasis. Which type of notes the clinician should record depends on the reason for the session. If the session's purpose is to address an identified problem, PIRP notes are most appropriate. If the session is to help the patient achieve a certain goal, the professional might opt for GIRP notes. If the session will allow the professional to better understand the patient, BIRP notes may be a better fit.
The clinician's choice of notes format will affect the treatment process. Sessions with an emphasis on problem-solving help a patient overcome a specific issue. On the other hand, sessions with an emphasis on achieving a goal help the patient appreciate milestones in their progress. And behavior-based notes allow a professional to determine the best course of action for each patient.
It's essential to understand various note formats and how they differ. Choosing the right note format can impact the treatment progression in vital ways. Keep in mind, every patient is unique, as is every circumstance. Different approaches work best for different patients. Clinical note examples will help you understand the format's impact.
PIRP Notes
PIRP notes are problem-focused. When writing PIRP notes, the healthcare professional focuses on a specific obstacle and documents their interventions, the patient's response to those interventions and the plan moving forward.
P: Problem
The "problem" could be a specific complaint, condition or reason for the present session. It's essentially a description of why the session is necessary. This section of the notes helps both the clinician and the patient understand why mental health intervention is applicable. A "problem" could be certain feelings, a substance use disorder or symptoms related to a diagnosis.
Within the "problem" section of the notes should be an assessment of the problem's current level. For instance, if the problem is depression symptoms, the professional will need to record the frequency and severity of those symptoms. They may also describe any progress or impairments to progress. They might determine whether or not a certain diagnosis is still valid.
I: Intervention
The "intervention" section of the notes should describe the treatment plan the professional has provided. It includes any recommendations or advice offered to the patient, including strategies for coping with, adapting to or solving the problem. The clinician should also discuss any skills they practiced or modeled with their patient.
R: Response
The "response" refers to the patient's response to the intervention — has the patient made progress toward resolving the problem? Has the patient experienced any hindrances in their progress? What reasons are there for a lack of improvement? In the response portion of the notes, the professional records the need for additional treatment. This section could include verbatim quotes from the patient.
P: Plan
In the "plan" portion of the notes, the clinician records the next steps for ongoing treatment. The plan might include:
- Follow-up items
- "Homework" for the patient
- Future treatment meetings
- Referrals to other resources
- New goals to set for the future
- Medication prescriptions
GIRP Notes
Goal-focused notes have to do with either short-term or long-term objectives and a patient's progression toward them. They differ from PIRP notes in that they focus on achieving a goal rather than solving a problem. GIRP-formatted notes are helpful for situations where a patient and healthcare provider have defined a clear goal together. It helps show the patient their ability to make small steps toward larger objectives, offering encouragement.
G: Goal
Notes on the "goal" include a description of the patient's current objective, whether long- or short-term. It's based on previous assessments or treatment plans. For instance, if a patient is in treatment for substance use disorder, an applicable goal may be to utilize learned coping skills three times per day. Another goal could be to identify three triggers.
I: Intervention
The "intervention" describes the professional's methods to propel the patient toward their goal. It should include details about approaches the clinician took and why. The intervention may include a facilitated discussion and the professional's suggestions.
R: Response
In GIRP notes, the "response" includes details about the patient's progress toward reaching the designated goal. It also describes the patient's overall attitude and behavior — if the patient appears guarded and withdrawn during the guided discussion, the observer will record this in the "response" part of the notes.
P: Plan
Based on the patient's response and any other information discovered during the session, the professional will determine a plan for the future. The plan should incorporate strategies for achieving short- and long-term goals. For instance, a plan could include:
- Attending future sessions
- A referral to another specialist
- Future discussion topics
BIRP Notes
BIRP notes are neither problem- nor goal-oriented. Instead, they describe the session's general theme and the patient's tone or attitude. BIRP notes place emphasis on the professional's observations and the patient's self-reported thoughts. Notes like these can be a good place to start concerning new patients or patients with less clear problems and goals.
B: Behavior
You might also see "behavior" as "presenting the problem." The "behavior" portion of the notes deals with the professional's observations of the patient and the patient's self-reported thoughts or feelings. As a clinical note example, the clinician may mention a patient's attitude during the session using words such as "withdrawn" or "engaged." They may also record direct quotes from the patient. Behavior-based notes could look something like this:
"During today's session, the patient showed signs of exhaustion and lack of focus. They said, 'I have not slept much during the past few nights. I'm feeling anxious and having trouble relaxing.'"
Notes might also include the professional's impression of the patient's attitude toward treatment. For example, they may mention a reluctance to engage in conversation or dismissal of new ideas.
As you can see, behavior-focused notes include both the clinician's observations and quotes from the patient. They do not outline a specific objective or concern. Instead, they discuss the client's general mood and appearance. Notes like these can be beneficial for a wide range of different patients, especially those who do not yet have a diagnosis or are beginning a new treatment plan.
I: Intervention
In BIRP notes, the "intervention" portion includes details about the session. It serves as a summary of the conversation and the professional's course of action. They may have asked the patient to identify any links between their insomnia and stressful situations in their day-to-day life, for instance. They might try to find connections between specific events and a lack of sleep.
The clinician will likely offer tools for addressing the discovered problems. They might suggest strategies for coping with stress, like social support, guided meditation or regular exercise. Any suggestions like these are examples of interventions, which the clinician should record in the patient's notes.
R: Response
Regarding BIRP notes, the patient's "response" has to do with their attitude toward interventions. The patient might be either pessimistic, optimistic or uncertain about a proposed intervention. For instance, a patient in treatment for a substance use disorder could mention feeling anxious about the possibility of a relapse but hopeful about trying new coping mechanisms. The professional should record direct quotes from the patient.
P: Plan
The plan for future treatment will depend on any revealed issues, as well as the patient's status. The plan might include:
- Identifying specific concerns or goals
- Scheduling future sessions
- Meeting with other professionals
- Starting or continuing medication
If further sessions are necessary, the clinician will describe the next session's goals or focus. They may want to take time to reassess certain attitudes or feelings or learn of a response to an intervention, for example.
Reducing Progress Note Documentation Time
Regardless of the type of notes a clinician chooses to write, note quality is always critical. Keeping accurate, chronological and understandable notes is a necessity. Quick and accurate notes can improve the treatment process.
The quality of a patient's notes will have a substantial impact on their ongoing treatment — sloppy or sparse notes might hinder treatment by breaking down communication between healthcare professionals. For instance, if a patient has to move and seek a new provider, they'll need detailed notes to avoid "starting over" their progression path. Here are some tips for writing clear, concise and quick progress notes:
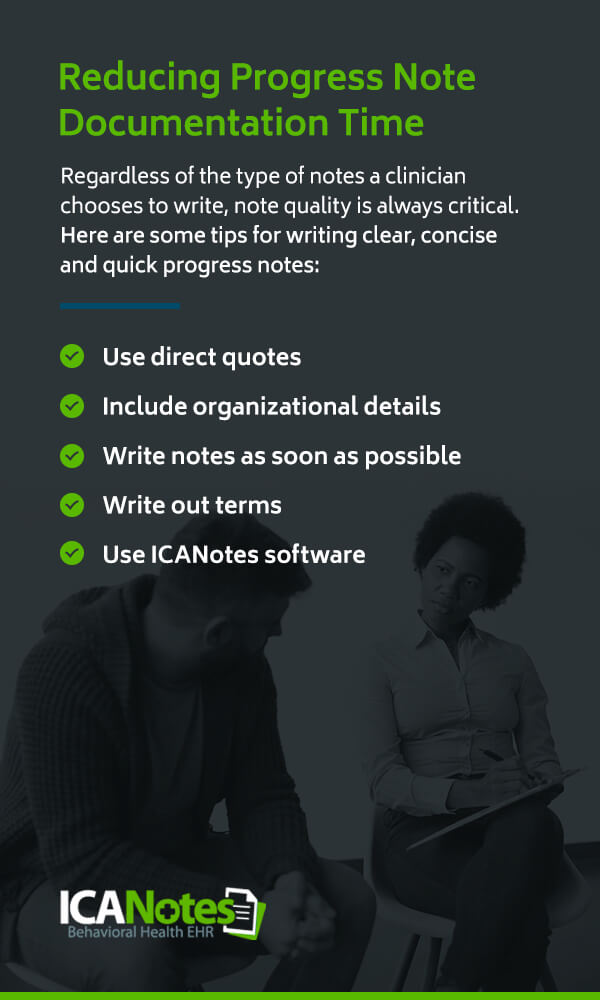
- Use direct quotes: Writing down direct quotes helps reduce subjectivity in the analysis. Patient quotes will help future healthcare providers understand the patient's state of mind.
- Include organizational details: Remember to write down record-keeping details such as the patient's full name and the session's date, time and duration. These pieces of information will help you keep your notes structured and chronological.
- Write notes as soon as possible: It's essential to write progress notes as soon as possible — during or immediately following a session. You may struggle to remember key details if you allow too much time to pass.
- Write out terms: While abbreviations can make writing notes faster in the moment, you should always spell them out to avoid future confusion.
- Use ICANotes software: Using a mental health note-recording software can make the process easier, simpler and quicker. Consider using ICANotes software to improve your progress notes.
How ICANotes Can Reduce Documentation Time
ICANotes offers pre-formatted content buttons to help you write better notes during sessions. Since minimal typing is necessary, the software will save you time and allow you to focus more attention on your patient. The ICANotes software tool offers all of the following features and benefits:
- It eliminates transcription expenses.
- It reduces the chance of misinterpretation from handwritten notes.
- It helps form an individualized narrative for each patient.
- It reduces documentation time.
- It offers protection from medical-legal liability.
- It gives you more flexibility to adjust notes from anywhere.
The ICANotes software will help you make patient treatment more streamlined and effective. Since the software is web-based, it's easy to implement without changing your current processes or altering your day-to-day operations. You can see the difference for yourself with the ICANotes free trial — give it a test run to see how it works for you. In addition to progress notes, the software can improve your:
- Initial assessments
- Group therapy notes
- Treatment plans
- Discharge summaries
Contact ICANotes to Learn More
Behavioral health services depend on full and accurate notes. Many different strategies and structures are available for note-recording, including PIRP, BIRP and GIRP. Each places emphasis on a different aspect of care — problem-solving, goal-setting or establishing observations. Regardless of the type of notes you prefer to write, making sure they're well-organized and easy-to-understand should always be a priority.
As a mental health specialist, improving your note writing capabilities allows you to offer your patients the best possible care. It'll help you determine a course of action, communicate with other specialists or healthcare providers and maintain a productive relationship with your patient. Proper note writing can also reduce legal liability and protect your practice.
ICANotes can help you write, organize and reference patient notes. The behavioral health documentation software reduces note-writing time. In addition to its note-related capabilities, ICANotes can help you with billing, charting, telehealth and other facets of mental health service. To learn more, contact us at ICANotes today.