Billing Pitfalls for Mental Health Clinicians
As a mental health clinician, you may have faced billing issues that add stress to your professional life. In comparison to other health care professionals, you may be at a disadvantage due to the types of services you offer and the pre-authorization needed. If your practice has been having a difficult time getting claims approved, you are not alone.
Mental health billing can get complicated, particularly due to the frequency of billing pitfalls. The services of psychiatrists, psychologists, counselors and therapists are provided in ways distinctly different from other health care professionals. Insurance companies can decide how long treatments are allowed to take and how many sessions can occur each day, making it challenging for mental health clinicians to balance successful billing with adequate patient treatment.
To help you with your billing, we have compiled this guide to help mental health clinicians identify and avoid common billing issues in healthcare.
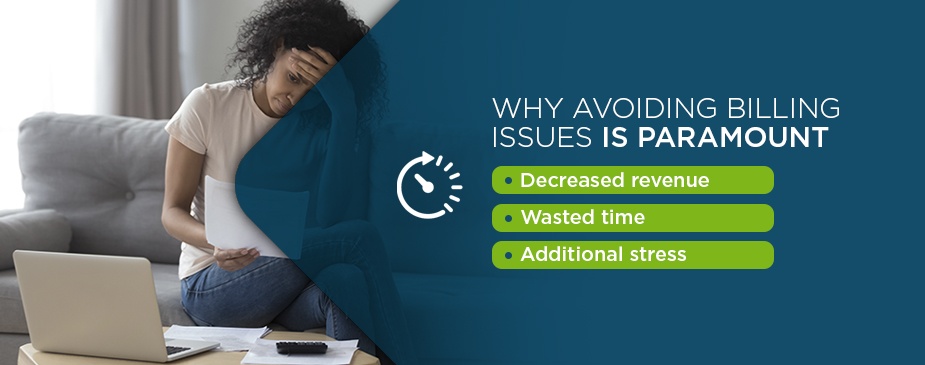
Why Avoiding Billing Issues Is Paramount
What do billing issues mean for mental health clinicians? Billing issues for mental health professionals can lead to:
- Decreased revenue
- Wasted time
- Additional stress
Figuring out how to balance serving clients with making time to address all administrative tasks can present a significant challenge to mental health clinicians.
While medical professionals tend to work in organizations with large office staffs who can handle claims and billing, mental health professionals typically work in practices with much smaller budgets and staffs. Billing generally falls to either a small office staff or on the therapist themselves. As such, many practices miss out on money that insurance companies owe them, with many collecting just 85% of what they are owed — or even less.
Billing is also different and more complex for mental health services than for medical billing because of the differences in standardization. If a patient visits his or her medical doctor, the doctor will likely perform standard tests and services, such as measuring a patient's weight and height, listening to a patient's heart, checking blood pressure and possibly drawing blood. These tests tend to be standardized across patients, differ only slightly between patients and take about the same amount of time. Thus, billing is also standardized and repetitive.
However, mental health services vary much more widely. The length of the session, the approach to therapy and the willingness of the patient to participate make it challenging to standardize treatment and billing. In fact, insurance companies have attempted to minimize payment through the standardization of mental health billing, which has led to restrictions on:
- How many treatments a patient can receive in a day or week.
- How long treatment can take.
- How many treatments can be covered.
Additionally, the requirement of pre-authorization has resulted in more difficulty and complexity for mental health billing. Fewer resources are available for providers of mental health care, and the clinicians themselves often shoulder the burden of billing, as many clinicians work in small group or solo practices with little administrative support.
Fortunately, with the right billing solution, you can improve your percentage of claims approvals and receive payments for claims more quickly.
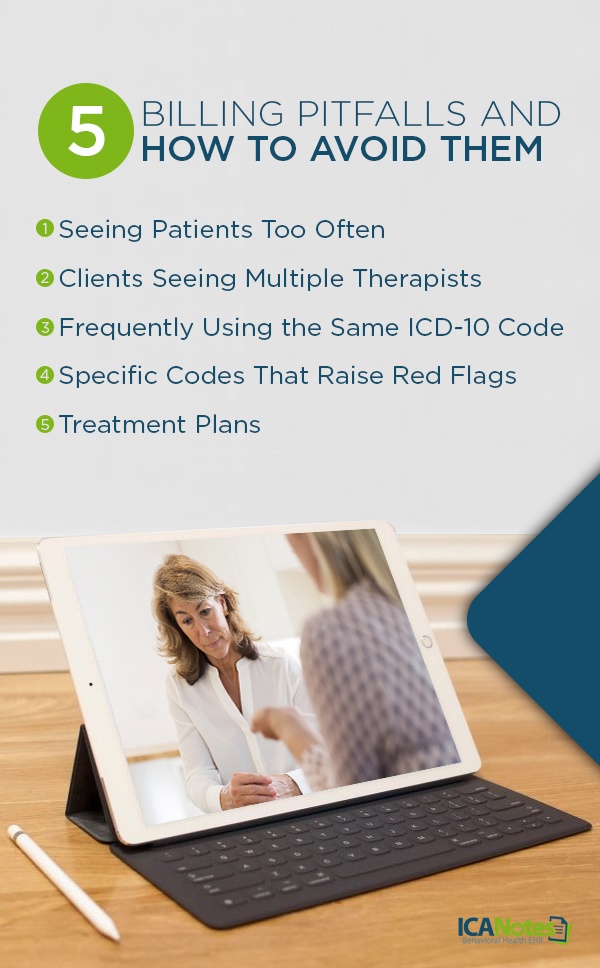
5 Billing Pitfalls and How to Avoid Them
As a mental health clinician, being paid for the services you deliver to patients is paramount. Unfortunately, due to the prevalence of insurance claim denials today, payment is not always guaranteed for your services. Payer sources use denials and rejections as tools to force clinicians to hand over hard-earned dollars.
Below, we have compiled a list of the five billing pitfalls you should know and avoid:
1. Seeing Patients Too Often
Seeing patients too often is one of the most common billing pitfalls. Seeing a patient once a week or every five to six days is standard, while seeing a patient three or more times a week is considered excessive. When a patient requires treatment more than once a week, then he or she should receive a higher level of care like Partial Hospitalization, IOP or inpatient admission.
Serving and billing a greater number of patients than you could feasibly see during a typical workday is another billing pitfall. For instance, seeing and billing 50 patients and using the same code for these patients may be a red flag to an insurance company. Similarly, if you work in a psych hospital for half of your workday and then are at a clinic for the second half of your workday where you claim to see 50 patients, this also is not considered feasible.
2. Clients Seeing Multiple Therapists
Another billing pitfall arises when a client is seeing multiple therapists. This situation can arise if a client must see a therapist in the same facility as his or her doctor, but he or she is also seeing a private therapist or counselor for personal reasons, such as if the client prefers sessions with the private therapist. A payer source will not want to pay for two different therapists for a single client.
To avoid this billing pitfall, discuss with your client why he or she is seeking therapy from another mental health professional. Is there a service the other therapist is offering that you could bring to the sessions? Additionally, make sure you only bill for the services you provide and only for the dates you treat the patient.
3. Frequently Using the Same ICD-10 Code
Using the same ICD-10 code too often is another common billing pitfall for mental health professionals. Variety is key in billing to avoid audit risk. When you bill the same diagnosis code for all of your patients, such as anxiety disorder, this is considered a red flag.
During the COVID-19 pandemic, insurance companies consider it acceptable to use the same code for a majority of patients. However, using the same code for each patient is not recommended or legal.
How can you avoid frequently using the same ICD-10 code? Document and stick to the evidence. Base your evaluation of a patient only on the data you have available and find the code that is as specific as possible. Acknowledge what you know, what you do not know and where you have gotten your information.
A problematic trend in mental health billing is overusing unspecified diagnosis codes. Using an unspecified code should be an exception, and a high rate of unspecified diagnosis codes could flag your practice for investigation. The following are conditions for which mental health professionals commonly use unspecified diagnosis codes to report:
- Alcohol use, abuse and dependence
- Drug use, dependence and abuse
- Depression
To reduce your risk of receiving a claim rejection, you should know which code to use and how it should be used. Try to find a code that is specific to the patient's condition. You should also be aware of how frequently you use an ICD-10 code and note any codes you may be using too often. Keep in mind that diversity is key in billing.
4. Specific Codes That Raise Red Flags
Additionally, another billing pitfall arises from the use of specific codes in mental health billing that can raise red flags. Billing too many specific codes for your services can create problems for your practice. Three of the codes to be aware of are 99215, 90837 and 90853.
- Billing code 90837 (individual psychotherapy): For 90837 codes, Medicare does not like seeing several occurrences of this code. Some mental health clinicians only bill this code, which will likely result in an audit. Additionally, a common issue with billing the 90837 code is that services performed must match the documentation.
- Billing code 99215 (established patient visit): Clinicians could also face pitfalls with the 99215 code. This code is used for medication management in worst-case scenarios. Though a payer source will reimburse clinicians for this code, it will become suspicious if you use this code for a patient several times in a row. A payer source wants to see billing completed on a bell curve.
- Billing code 90853 (group psychotherapy): Additionally, billing 90853 needs to be executed carefully. Make sure everyone in the caseload is marked in attendance and documented in the group therapy session. Because the clinician is billing several patients at once, billing this code can be challenging. To avoid an audit, your documentation should be precise and accurate, particularly for drug addiction groups.
Use the proper code based on the time spent with the patient in the therapy session. For example, if a treatment lasted 15 minutes, you should not use a code that represents one hour of treatment.
How can you avoid raising red flags with these specific codes? The key is understanding the codes. Insurance companies use common procedural technology codes to decide what amount of reimbursement should be given to a health care facility. Knowing which codes are associated with the services you offer will help you ensure billing accuracy.
If you use the codes 90837, 99215 and 90853, you should be aware that they can raise red flags with insurance companies and make sure that you are taking all necessary steps to avoid billing issues with these codes.
5. Treatment Plans
The final billing pitfall for mental health professionals lies in treatment plans for patients. Not completing a treatment plan is a sure way to not receive payment or to be required to pay back money to a payer source after an audit.
Some agencies mandate that a treatment plan be signed by the patient. If the plan is not signed, then you would need to forfeit funds. Additionally, in completing treatment plans, mental health professionals have attempted to bill 90833 or 90836 for extra time. However, because this extra time constitutes therapy, a treatment plan is needed.
Documentation and billing errors can occur when a claim is missing progress notes and does not include a plan for the patient's long-term care. Your documentation should include:
- Encounter notes
- Timesheets
- Details about the place and time of service
- Evidence that a treatment plan was developed by a professional team, the patient and the patient's family
Ensure that documentation also includes any allergies the patient has. An insurance company does not want a blank space. If a patient has no known allergies, this should be stated within the documentation.
Innovative Charting Solutions for Billing
Robust and advanced charting solutions or a templated EHR can make documentation quick and easy, preventing prospective billing issues. At ICANotes, we offer our customers a fully templated EHR. We deliver an intuitive and robust charting solution for both inpatient and outpatient settings.
Why do our customers choose us for billing? At ICANotes, behavioral health organizations and clinicians turn to us in the following scenarios:
- When they are dedicating too many hours to producing documentation.
- When they are losing money due to claims being rejected or notes being under-coded.
- When they feel frustrated by the turnaround time and expense of transcribing clinical dictation.
- When they are unsure whether their documentation will be able to pass regulatory scrutiny.
- When their job has become more stressful and difficult than ever due to the growing complexity of the industry.
- When they are looking to combine charting with practice management and electronic billing via our integrated behavioral health software solution.
Our templated EHR is ready out of the box. This solution can make your behavioral health documentation fast, sophisticated and comprehensive enough to meet the required standards. You will not have to worry about dedicating lots of time to training, as our templated EHR is highly intuitive and includes a chart-centric workflow that is clinically logical.
Our product was developed by clinicians who have a thorough understanding of behavioral health. Our EHR software essentially thinks like a clinician, which means it will provide you with the benefits and billing solutions you are seeking.
Try ICANotes for EHR-Integrated Billing Software
With ICANotes, you can bill the way you choose. Select the option that works best for the needs of your practice. Our integrated solution will allow you to streamline your billing and receive payments faster. Create CMS forms, statements and superbills with a comprehensive system. Use the integrated card processing system we offer or take check and cash payments.
Our mental health billing software can offer you the following benefits:
- Enjoy secure data management.
- Choose from a variety of clearinghouse solutions.
- Receive assistance with revenue cycle management.
By improving your billing with our comprehensive solutions, you can enhance the standard of care and operations in your practice. To learn more about our EHR-integrated billing software, contact us at ICANotes or request a free trial today.
Sources
- https://bpsbilling.com/resources/how-is-mental-health-billing-different-from-medical-billing/
- https://www.counseling.org/news/aca-blogs/aca-member-blogs/aca-member-blogs/2012/12/17/mental-health-billing-10-common-questions-and-answers
- https://fixmyclaim.com/3-tips-for-mental-and-behavioral-health-billing/
- https://library.ahima.org/doc?oid=302473#.XuD8WJ5KjBI
- https://www.icanotes.com/features/billing/
Related Posts
CPT Code Basics: What You Should Know
How to Prepare for an Insurance Treatment Review
Mental & Behavioral Healthcare Billing: How to Maximize Your Reimbursement Rate